Մասնակից:LianaYeghiazaryan/Ավազարկղ
Վիրուսային մենինգիտ
[խմբագրել | խմբագրել կոդը]| Վիրուսային մենինգիտ | |
|---|---|
 Վիրուսային մենինգիտը ուղեղային պատյանների բորբոքման պատճառ է |
Վիրուսային մենինգիտ (հայտնի նաև որպես ասեպտիկ մենինգիտ) մենինգիտի տարատեսակ է, որը առաջանում է վիրուսային վարակի հետևանքով։ Այն հանդիսանում է ուղեղային պատյանների բորբոքման արդյունք (այդ պատյանները պատում են գլխուղեղն և ողնուղեղը)։ Ախտանշաններն ընդգրկում են գլխացավ, տենդ, լուսավախություն և պարանոցի կարկամություն[1]։
Վիրուսները ասեպտիկ մենինգիտնի ամենատարացված պատճառներից մեկն են[2]։ Վիրուսային մենինգիտների առաջացման մեծ մասն են կազմում Էնտերովիրուսները[3][4][5]: Սակայն այլ վիրուսները նույնպես կարող են վիրուսային մենինգիտ առաջացնել։ Օրինակ՝ Արևմտյան Նիլի վիրուսը, խոզուկի, կարմրուկի, Հերպես Սիմպլեքս 1, 2, գոտևորող հերպեսի, ավշային հորեոմենինգիտի վիրուսները[6]։ Կլինիկական ախտանիշների հիման վրա հնարավոր չէ լիարժեք տարբերակել բակտերիալ մենինգիտից, չնայած վիրուսային մենինգիտի դասական կլինիկայի ընթաքցքը ավելի թեթև է։ Վիրուսային մենինգիտի դեպքում ուղեղ-ողնուղեղային հեղուկում բակտերիաները բացակայում են։ Հետևաբար հիվանդությունը հաստատելու համար հաճախ անհրաժեշտ է կատարել գոտկային պունկցիան ուղեղ-ողնուղեղային հեղուկի անալիզով[7]։
Դեպքերի մեծ մասը հատուկ բուժում չի պահանջում և բոլոր ջանքերն ուղղված են սիմպտոմատիկ բուժման (գլխացավի, տենդի, սրտխառնոցի վերացմանը)[8]։ Որոշ վիրուսների դեպքում պահանջ կա հատուկ բուժման, օրինակ՝ Հերպես սիմպլեքս վիրուսի դեպքում։
ԱՄՆ-ում մենինգիտների կեսից ավել դեպքերի պատճառ է վիրուսային մենինգիտը[9]։ 1988-1999 թվականների ընթացքում յուրաքանչյուր տարի 36․000 դեպք է գրանցվել[10]։ Հիվանդանում են մեծահասակները և երեխաները, բայց ավելի շատ հիվանդությունը տարածված է երեխաների մոտ[1]։
Նշաններ և ախտանիշներ
[խմբագրել | խմբագրել կոդը]Վիրուսային մենինգիտին բնորոշ են տենդ, գլխացավ, պարանոցի կարկամություն[11]։ Տենդը ցիտոկինների արտազատման արդյունք է, որոնք ազդում են հիպոթալամուսի ջերմակարգավորիչ նեյրոնների վրա: Ցիտոկինները և բարձրացած ներգանգային ճնշումը խթանում են գլխուղեղի ցավի ընկալիչները (նոցիցեպտորները)` առաջացնելով գլխացավ: Պարանոցի կարկամությունը ողնաշարի ծալվելու ժամանակ բորբոքված ուղեղային թաղանթների ձգման արդյունք է[12]։ Ի տարբերություն բակտելիալ մենինգիտի՝ հիվանդության ախտանիշները հաճախ ավելի թեթև են և ավելի դանդաղ են զարգանում[11]։ Սրտխառնոցը, փսխումը և լուսավախությունը նույնպես ի հայտ են գալիս ընդհանուր վիրուսային մենինգիտին բնորոշ նշանների հետ միասին, որոնք են մկանային ցավն եվ ընդհանուր թուլությունը[11]։ Բարձրացած ներգանգային ճնշումը խթանում է Area postrema, որն իր հերթին առաջացնում է սրտխառնոց և փսխում: Լուսավախությունը կապված է ուղեղային պատյանների գրգռման հետ[12]։ Ծանր դեպքերում կարող է զարգանալ էնցեֆալիտ (մենինգոէնցեֆալիտ) հետևյալ ախտանիշաններով՝ ցնցումներ, օջախային նյարդաբանական դեֆիցիտներ և փոփոխված մտավոր կարգավիճակ[13]։
Փոքր երեխաների մոտ վիրուսային մենինգիտը կարող է դրսևորվել միայն գրգռվացությամբ, քնկոտությամբ կամ սնվելու հետ կապված խնդիրներով[7]։ Ծանր դեպքերում կարող է զարգանալ էնցեֆալիտ (մենինգոէնցեֆալիտ) հետևյալ ախտանիշաններով՝ ցնցումներ, օջախային նյարդաբանական դեֆիցիտներ և փոփոխված մտավոր կարգավիճակ[13]։ Երեխաների մոտ կարող են ի հայտ գալ որոշ լչացուցիչ ախտանիշներ,որոնք ներառում են դեղնախտ և գաղթունի արտափքում[12]։
Ախտածագում
[խմբագրել | խմբագրել կոդը]ԱՄՆ-ում վիրուսային մենինգիտի ամենատարածված պատճառ ոչ-պոլիո էնտերովիրուսներ են: Մենինգիտ առաջացնող վիրուսներ սովորաբար փոխանցվում են հիվանդների հետ շփվելիս:Այնուամենայնիվ, շատ դեպքերում այն մարդկանց մոտ որոնք վարակված են մենինգիտ առաջացնող վիրուսներով , մենինգիտ չի զարգանում[7]։
Վիրուսներն, որոնք կարող են մենինգիտի առաջացման պատճառ հանդիսանալ[14]։
- Էնտերովիրուսներ
- Էնտերովիրուս 71
- Էխովիրուս
- Պոլիովիրուս (PV1, PV2, PV3)
- Կոկսակի A վիրուս (CAV); նաև Ձեռք ոտք բերան հիվանդություն
- Հերպես վիրուսներ (HHV)
- Հերպես սիմպլեքս վիրուս տիպ 1 (HSV-1 / HHV-1) կամ տիպ 2 (HSV-2 / HHV-2); նաև պատճառ է բերանային հերպեսի կամ գենիտակ հերպեսի
- Վարիցելա զոստեր (VZV / HHV-3); նաև առաջացնում է ջրծաղիկ և Գոտևորող որքին (հերպես զոստեր)
- Էպշտեյն-Բարի վիրուս (EBV / HHV-4); նաև առաջացնում է Ինֆեկցիոն մոնոնուկլեոզ/"մոնո"
- Ցիտոմեգալովիրուս (CMV / HHV-5)
- Մարդու իմունային անբավարարության վիրուս (ՄԻԱՎ); [[]]
- Լա Կրոսսե վիրուս
- Լիմֆոցիտային խորեոմենինգիտի վիրուս (LCMV)
- Կարմրուկ
- Խոզուկ
- Սբ․Լուիս էնցեֆալիտի վիրուս
- Արևմտյան Նիլի վիրուս
Մեխանիզմ
[խմբագրել | խմբագրել կոդը]Վիրուսային մենինգիտը հիմնականում առաջանում է վարակային ագենտով, որը գաղութ է առաջացնում իր տիրոջ որևէ մասում[15]։ Իմունոդեֆիցիտ ունեցող հիվանդները ամենաբարձր ռիսկի խումբ են համարվում հարուցիչի ներխուժման համար[12]։ Վարակման ուղիներն են՝ մաշկը, շնչառական ուղի, աղեստամոքսային ուղի, քթըմպանն և միզասեռական համակարգ։ Վիրուսը ներխուժում է տիրոջ ենթալորձային շերտ պաշտպանիչ շերտի միջոցով, ինչպիսիք են՝ տեղային իմունիտետը, ֆիզիկական պատնեշնեշը, ֆագոցիտները և մակրոֆագերը[15]։ Ներթափանցումից հետո իմունային համակարգը ակտիվանում է[12]։ Վարակիչ ագենտը կարող է թափանցել կենտրոնական նյարդային համակարգ և առաջացնել մենինգիտ երեք ճանապարհով, որոնք են՝ հեմատոգեն,ռետրոգրադ նյարդային ճանապարհով կամ ուղղակի մերձակից միջոցով[16]։ Իմուն բջիջները և վնասված էնդոթելիալ բջիջները արտազատում են մատրիքսային մետալոպրոտեինազներ (ՄՄՊ-ներ), ցիտոկիններ և ազոտի մոնոօքսիդ (NO): ՄՄՊ-ները և NO անոթալայնիչ ազդեցություն ունեն գլխուղեղի անոթներում: Ցիտոկիններն առաջացնում են մազանոթային պատի փոփոխություններ արյուն-ուղեղային պատնեշում (ԱՈւՊ), ինչն իր հերթին հանգեցնում է լեյկոցիտների ռեցեպտորների էքսպրեսիայի խթացման՝ բարձրացնելով սպիտակ արյան բջիջների կպումը և էկստրավազացիան[12]։ Պատնեշը, որը ստեղծված է ուղեղի և արյան հոսքի միջև ուղեղային պատյաններով, նորմայում պաշտպանում է ուղեղը մարմնի իմունային համակարգից: Ուղեղային պատյանների և էնդոթելիալ բջիջների վնասումը բարձրացնում է թթվածնի ցիտոտոքսիկ ռեակտիվ տեսակների առաջացումը, որոնք վնասում են վարակիչ ագենտին և հարևան բջիջներին[12]։ Մենինգիտի դեպքում պատնեշը վնասված է. վիրուսները, թափանցելով ուղեղ, մեկուսացված են իմուն համակարգից և կարող են տարածվել[17]։ Այն բերում է ներգանգային ճնշման բարձրացման, ուղեղի այտուցի, մենինգեալ գրգռվածության և նեյրոնների մահվան[12]։
Ախտորոշում
[խմբագրել | խմբագրել կոդը]Վիրուսային մենինգիտի ախտորոշումը կատարվում է կլինիկական պատմության, ֆիզիկական զննման և որոշ ախտորոշիչ թեստերի հիման վրա[18]։ Շատ կարևոր է անել ուղեղ-ողնուղեղային հեղուկի (ՈւՈՀ) հավաքում գոտկային պունկցիայի միջոցով:Այս հեղուկը, որը նորմայում շրջապատում է ուղեղը և ողնուղեղը, անալիզի են ենթարկվում՝ փնտրելով վարակի նշաններ[19]։ ՈւՈՀ- ի նշանները, որոնք ցույց են տալիս մենինգիտի վիրուսային ախտածագումը, ներառում են սպիտակ արյան բջիջների բարձր քանակություն (սովորաբար 10-100 բջիջ /մլ )՝ լիմֆոցիտների գերակշռությամբ համադրվում է գլյուկոզի նորմալ կոնցենտրացիայի հետ[20]։ ՈՒՈՀ-ի ՊՇՌ թեստերը հատկապես օգտակար են դարձել վիրուսային մենինգիտի ախտորոշման համար (զգայնությունը կազմում է 95-100%) [21]։ Հավելյալ քղանքի, մեզի, արյան անալիզների և կոկորդից քսուքի պատասխանները նույնպես օգնում են հայտնաբերել վիրուսային մենինգիտը[19]։
Որոշ դեպքերում թույլ իմունային համակարգ կամ բարձրացած ներգանգային ճնշում ունեցող անձանց մոտ ուղեղի Համակարգչային շերտագրություն արվում է գոտկային պունկցիայից առաջ[1]։
Բուժում
[խմբագրել | խմբագրել կոդը]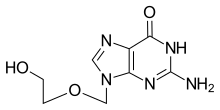
Բուժումը հիմնականում աջակցող է: Հանգիստ, հիդրատացիա, ջերմիջեցնողները, ցավազրկողները և հակաբորբոքային դեղերը տրամադրվում են եթե անհրաժեշտ է[22]։ Հերպես սիմպլեքս վիրուսը, Վարիցելա զոոստեր վիրուսը և Ցիտոմեգալովիրուսը պահանջում են հատուկ հակավիրուսային։ Օրինակ՝ Հերպես վիրուսի համար օգտագործում են Ացիկլովիր[23]։ Արագ բարձրացող ներգանգային ճնշման, ոսկրային կառույցի մոտ վարակի առկայության (մաստոիդիտի դեպքում), գանգի կոտրվածքի կամ աբսցեսի առաջացման դեպքերում անհրաժեշտ է վիրաբուժական բուժում[12]։ Վիրուսային մենինգիտ ունեցող մարդկանց մեծամասնությունը լավանում են 7-ից 10 օրերի ընթացքում[24]։
Համաճարակաբանություն
[խմբագրել | խմբագրել կոդը]1988-1999 թվականների ընթացքում յուրաքանչյուր տարի 36․000 դեպք է գրանցվել[25]։ Հիվանդանում են մեծահասակները և երեխաները, բայց ավելի շատ հիվանդությունը տարածված է երեխաների մոտ[1]։ Ռումինյայում և Իսպանիայում տեղի ունեցած բռնկումների ժամանակ վիրուսային մենինգիտը ավելի շատ տարածված էր մեծահասակների մոտ[26]։ Մինչդեռ 15 տարեկանից ցածր պատանիների մոտ դեպքերի տոկոսը կազմում էր 33․8 %[26]: Այլ պատկեր էր Ֆինլյանդիայում (1966թ.), Կիպրոսում (1996թ.), Ղազայում (1997թ.), Չինաստանում (1998թ.) և Թայվանում (1998թ.), որտեղ վիրուսային մենինգիտը ավելի շատ տարածված էր երեխաների, մանուկների մոտ[27][28][29][30]։
Վաղ հետազոտություններ
[խմբագրել | խմբագրել կոդը]Կա ենթադրություն, որ վիրուսային մենինգիտը կարող է հանգեցնել ողնաշարային զարկերակի բորբոքային վնասմանը[31]։
Մենինգիտի Հետազոտման Հիմնադրամը կատարում է հետազոտություն, որի նպատակը գենային տեխնոլոգիաների միջոցով մենինգիտի ախտորոշման արագությունը բարելավվելն է, ճշգրտությունը և մատչելիությունը երեխաների մոտ Մեծ Բրիտանիայում: Հետազոտական խումբը զարգացնում է նոր մեթոդներ, որոնք օգտագործվելու են մենինգիտի ախտորոշման համար՝ հետազոտելով ՈՒՈՀ-ում հայտնված միկրոօրգանիզմների գենետիկ մատերիալը։ Նոր մեթոդը նախ և առաջ պետք է կիրառվի՝ օգտագործելով ՈւՈՀ-կի նմուշներ, որտեղ միկրոօրգանիզմը հայտնի է, այնուհետև կիրառվի՝ օգտագործելով ՈՒՈՀ-կի նմուշներ, որտեղ միկրոօրգանիզմը անհայտ է (գնահատվում է մոտ 40%) փորձելով բացահայտել պատճառը[32]։
Ծանոթագրություններ
[խմբագրել | խմբագրել կոդը]- ↑ 1,0 1,1 1,2 1,3 Logan, SA; MacMahon, E (5 January 2008). «Viral meningitis». BMJ (Clinical research ed.). 336 (7634): 36–40. doi:10.1136/bmj.39409.673657.ae. PMC 2174764. PMID 18174598.
- ↑ «Aseptic Meningitis». Healthline (անգլերեն). Վերցված է 10 March 2017-ին.
- ↑ «Epidemiology». Alaska Department of Health and Social Services.
- ↑ Logan, SA; MacMahon, E (Jan 5, 2008). «Viral meningitis». BMJ (Clinical research ed.). 336 (7634): 36–40. doi:10.1136/bmj.39409.673657.ae. PMC 2174764. PMID 18174598.
- ↑ Ratzan, K. R. (1985-03-01). «Viral meningitis». The Medical Clinics of North America. 69 (2): 399–413. doi:10.1016/s0025-7125(16)31051-3. ISSN 0025-7125. PMID 3990441.
- ↑ «Acute Communicable Disease Control». lacounty.gov.
{{cite web}}:|first1=missing|last1=(օգնություն) - ↑ 7,0 7,1 7,2 «Meningitis | Viral | CDC». www.cdc.gov (ամերիկյան անգլերեն). Վերցված է 2017-03-02-ին.
- ↑ «Viral Meningitis - Meningitis Research Foundation». www.meningitis.org. Վերցված է 2017-03-02-ին.
- ↑ Bartt, R (December 2012). «Acute bacterial and viral meningitis». Continuum (Minneapolis, Minn.). 18 (6 Infectious Disease): 1255–70. doi:10.1212/01.CON.0000423846.40147.4f. PMID 23221840.
- ↑ Khetsuriani, N; Quiroz, ES; Holman, RC; Anderson, LJ (Nov–Dec 2003). «Viral meningitis-associated hospitalizations in the United States, 1988–1999». Neuroepidemiology. 22 (6): 345–52. doi:10.1159/000072924. PMID 14557685.
- ↑ 11,0 11,1 11,2 «Viral Meningitis - Brain, Spinal Cord, and Nerve Disorders - Merck Manuals Consumer Version». Merck Manuals Consumer Version (ամերիկյան անգլերեն). Վերցված է 2017-03-04-ին.
- ↑ 12,0 12,1 12,2 12,3 12,4 12,5 12,6 12,7 12,8 «Meningitis | McMaster Pathophysiology Review». www.pathophys.org (ամերիկյան անգլերեն). Վերցված է 2017-12-12-ին.
- ↑ 13,0 13,1 Cho, Tracey A.; Mckendall, Robert R. (2014-01-01). Booss, Alex C. Tselis and John (ed.). Handbook of Clinical Neurology. Neurovirology. Vol. 123. Elsevier. էջեր 89–121.
- ↑ Meningitis 1168529, բաժին Viral Meningitis(անգլ.) EMedicine կայքում
- ↑ 15,0 15,1 «Viral Meningitis: Background, Pathophysiology, Etiology». 2017-11-29.
{{cite journal}}: Cite journal requires|journal=(օգնություն) - ↑ Klimpel, Gary R. (1996). Baron, Samuel (ed.). Medical Microbiology (4th ed.). Galveston (TX): University of Texas Medical Branch at Galveston. ISBN 0963117211. PMID 21413332.
- ↑ Chadwick, D. R. (2005-01-01). «Viral meningitis». British Medical Bulletin (անգլերեն). 75–76 (1): 1–14. doi:10.1093/bmb/ldh057. ISSN 0007-1420.
- ↑ «Diagnosis - Meningitis - Mayo Clinic». www.mayoclinic.org (անգլերեն). Վերցված է 2017-03-04-ին.
- ↑ 19,0 19,1 «CSF analysis: MedlinePlus Medical Encyclopedia». medlineplus.gov (անգլերեն). Վերցված է 2017-03-04-ին.
- ↑ «CSF Analysis - Neurology - UMMS Confluence». wiki.umms.med.umich.edu. Վերցված է 2017-03-04-ին.
- ↑ Fomin, Dean A. Seehusen|Mark Reeves|Demitri. «Cerebrospinal Fluid Analysis - American Family Physician». www.aafp.org (անգլերեն). Վերցված է 2017-03-04-ին.
- ↑ «Viral Meningitis Treatment & Management: Approach Considerations, Pharmacologic Treatment and Medical Procedures, Patient Activity». 2017-11-29.
{{cite journal}}: Cite journal requires|journal=(օգնություն) - ↑ Tyler KL (June 2004). «Herpes simplex virus infections of the central nervous system: encephalitis and meningitis, including Mollaret's». Herpes. 11 (Suppl 2): 57A–64A. PMID 15319091.
- ↑ «Meningitis | Viral | CDC». www.cdc.gov (ամերիկյան անգլերեն). 2017-12-04. Վերցված է 2017-12-11-ին.
- ↑ Khetsuriani, N; Quiroz, ES; Holman, RC; Anderson, LJ (Nov–Dec 2003). «Viral meningitis-associated hospitalizations in the United States, 1988–1999». Neuroepidemiology. 22 (6): 345–52. doi:10.1159/000072924. PMID 14557685.
- ↑ 26,0 26,1 Jiménez Caballero, PE; Muñoz Escudero, F; Murcia Carretero, S; Verdú Pérez, A (Oct 2011). «Descriptive analysis of viral meningitis in a general hospital: differences in the characteristics between children and adults». Neurologia (Barcelona, Spain). 26 (8): 468–73. doi:10.1016/j.nrleng.2010.12.004. PMID 21349608.
- ↑ Rantakallio, P; Leskinen, M; von Wendt, L (1986). «Incidence and prognosis of central nervous system infections in a birth cohort of 12,000 children». Scandinavian journal of infectious diseases. 18 (4): 287–94. doi:10.3109/00365548609032339. PMID 3764348.
- ↑ «1998—Enterovirus Outbreak in Taiwan, China—update no. 2». WHO.
- ↑ «1997—Viral meningitis in Gaza». WHO.
- ↑ «1996—Viral meningitis in Cyprus». WHO.
- ↑ Pan, Xudong. «Vertebral artery dissection associated with viral meningitis». BMC Neurology. 12.
- ↑ «Using new genomic techniques to identify the causes of meningitis in UK children | Meningitis Research Foundation». www.meningitis.org. Վերցված է 2017-12-12-ին.
External links
[խմբագրել | խմբագրել կոդը]| Դասակարգում | |
|---|---|
| Արտաքին աղբյուրներ |
Կաղապար:Viral diseases Կաղապար:Diseases of meninges
Կաղապար:Pp-protected Կաղապար:Use dmy dates Կաղապար:Infobox medical condition (new) Lyme disease, also known as Lyme borreliosis, is an infectious disease caused by a bacteria named Borrelia spread by ticks.[1] The most common sign of infection is an expanding area of redness on the skin, known as erythema migrans, that appears at the site of the tick bite about a week after it occurred.[2] The rash is typically neither itchy nor painful.[2] Approximately 70-80% of infected people develop a rash.[2] Other early symptoms may include fever, headache and tiredness.[2] If untreated, symptoms may include loss of the ability to move one or both sides of the face, joint pains, severe headaches with neck stiffness, or heart palpitations, among others.[2] Months to years later, repeated episodes of joint pain and swelling may occur.[2] Occasionally, people develop shooting pains or tingling in their arms and legs.[2] Despite appropriate treatment, about 10 to 20% of people develop joint pains, memory problems, and tiredness for at least six months.[2][3]
Lyme disease is transmitted to humans by the bite of infected ticks of the genus Ixodes.[4] In the United States, ticks of concern are usually of the Ixodes scapularis type, and must be attached for at least 36 hours before the bacteria can spread.[5][6] In Europe ticks of the Ixodes ricinus type may spread the bacteria more quickly.[6][7] In North America, Borrelia burgdorferi and Borrelia mayonii are the cause.[1][8] In Europe and Asia, the bacteria Borrelia afzelii and Borrelia garinii are also causes of the disease.[1] The disease does not appear to be transmissible between people, by other animals, or through food.[5] Diagnosis is based upon a combination of symptoms, history of tick exposure, and possibly testing for specific antibodies in the blood.[9][10] Blood tests are often negative in the early stages of the disease.[1] Testing of individual ticks is not typically useful.[11]
Prevention includes efforts to prevent tick bites such as by wearing clothing to cover the arms and legs, and using DEET-based insect repellents.[1] Using pesticides to reduce tick numbers may also be effective.[1] Ticks can be removed using tweezers.[12] If the removed tick was full of blood, a single dose of doxycycline may be used to prevent development of infection, but is not generally recommended since development of infection is rare.[1] If an infection develops, a number of antibiotics are effective, including doxycycline, amoxicillin, and cefuroxime.[1] Standard treatment usually lasts for two or three weeks.[1] Some people develop a fever and muscle and joint pains from treatment which may last for one or two days.[1] In those who develop persistent symptoms, long-term antibiotic therapy has not been found to be useful.[1][13]
Lyme disease is the most common disease spread by ticks in the Northern Hemisphere.[14] It is estimated to affect 300,000 people a year in the United States and 65,000 people a year in Europe.[1][15] Infections are most common in the spring and early summer.[1] Lyme disease was diagnosed as a separate condition for the first time in 1975 in Old Lyme, Connecticut.[16] It was originally mistaken for juvenile rheumatoid arthritis.[16] The bacterium involved was first described in 1981 by Willy Burgdorfer.[17] Chronic symptoms following treatment are well described and are known as post-treatment Lyme disease syndrome (PTLDS).[13] PTLDS is different to chronic Lyme disease; a term no longer supported by the scientific community and used in different ways by different groups.[13] Some healthcare providers claim that PTLDS is caused by persistent infection, but this is not believed to be true because of the inability to detect infectious organisms after standard treatment.[18] A vaccine for Lyme disease was marketed in the United States between 1998 and 2002, but was withdrawn from the market due to poor sales.[1][19] Research is ongoing to develop new vaccines.[1]
Signs and symptoms
[խմբագրել | խմբագրել կոդը]
Lyme disease can affect multiple body systems and produce a broad range of symptoms. Not all patients with Lyme disease have all symptoms, and many of the symptoms are not specific to Lyme disease, but can occur with other diseases, as well. The incubation period from infection to the onset of symptoms is usually one to two weeks, but can be much shorter (days), or much longer (months to years).[21]
Symptoms most often occur from May to September, because the nymphal stage of the tick is responsible for most cases.[21] Asymptomatic infection exists, but occurs in less than 7% of infected individuals in the United States.[22] Asymptomatic infection may be much more common among those infected in Europe.[23]
Early localized infection
[խմբագրել | խմբագրել կոդը]Early localized infection can occur when the infection has not yet spread throughout the body. Only the site where the infection has first come into contact with the skin is affected. The classic sign of early local infection with Lyme disease is a circular, outwardly expanding rash called erythema migrans (EM), which occurs at the site of the tick bite three to 32 days after the tick bite.[1] The rash is red, and may be warm, but is generally painless. Classically, the innermost portion remains dark red and becomes indurated (thicker and firmer), the outer edge remains red, and the portion in between clears, giving the appearance of a bull's eye, known as a target lesion. However, partial clearing is uncommon, and the bull's-eye pattern more often involves central redness.[1]
The EM rash associated with early infection is found in about 70–80% of people infected.[2] It can have a range of appearances including the classic bull's-eye pattern and non-target appearing lesions. The 20–30% without the EM and the non-target lesions can often cause misidentification of Lyme disease.[24] Affected individuals can also experience flu-like symptoms, such as headache, muscle soreness, fever, and malaise.[25] Lyme disease can progress to later stages even in people who do not develop a rash.[23][26]
Early disseminated infection
[խմբագրել | խմբագրել կոդը]Տեղային վարակի սկզից մի քանի շաբաթ հետո,Բորելիա բակտերիա կարող է սկսել տարածվել արյան հոսքով։ Within days to weeks after the onset of local infection, the Borrelia bacteria may begin to spread through the bloodstream.Թափառող էրիթեմա կարող է զարգանալ մարմնի այն մասերում,որը չի առնչվում տզի խայթման առաջնային տեղամասի հետ հետ։ EM may develop at sites across the body that bear no relation to the original tick bite.[27] Մաշկի այլ դրսևորում, որը բացակայում է հիվանդների մոտ Հյուսիսային Ամերիկայում ,բայց առկա է Եվրոպայում բորելիոզ լիմֆոցիտոմա է `մանուշակագույն զանգված ,որը զարգանում է ականջի,պտուկների կամ։ Another skin condition, apparently absent in North American patients, but found in Europe, is borrelial lymphocytoma, a purplish lump that develops on the ear lobe, nipple, or scrotum.[28] Տարատեսակ սուր նյարդաբանական խնդիրներ, որոնք կոչվում են նեյրոբորելիոզ զարգանում են չբուժված հիվանդների մոտ 10-15%։Various acute neurological problems, termed neuroborreliosis, appear in 10–15% of untreated people.[25][29] Ներառում են դիմային նյարդի պարալիզ,որը դեմքի միակողմանի կամ երկողմանի մկանային տոնուսի կորուստ է,որը մենինգիտի պես ներառում է ուժեղ գլխացավ,պարանոցի կարկամություն և լուսավախություն։These include facial palsy, which is the loss of muscle tone on one or both sides of the face, as well as meningitis, which involves severe headaches, neck stiffness, and sensitivity to light. Ողնուղեղային նյարդերի արմատների բորբոքումը կարող են պատճառ դառնան կրակող ցավի,որոնք խանգարում են քնելուն։,նույնպես ,ինչպես մաշկի փոփոխված զգայնությունը Inflammation of the spinal cord's nerve roots can cause shooting pains that may interfere with sleep, as well as abnormal skin sensations.Թեթև էնցեֆակիտը կարող է բերել հիշողության կորստի,քնի խանգարումների կամ տրամադրության փոփոխությանը։ Mild encephalitis may lead to memory loss, sleep disturbances, or mood changes.Որոշ դեպքերում զեկուցվում է փոփոխված հոգեկան վիճակի մասին որպես վաղ նեյրոբորելիոզի միակ ախտանիշ։ In addition, some case reports have described altered mental status as the only symptom seen in a few cases of early neuroborreliosis.[30] Հիվանդությունը կարող է ազդել սրտի հաղորդչական համակարգի վրա և կարող է անկանոն սրթտի ռիթմի պատճառ դառնալ ,ինչպես օրինակ նախասիրտ-փորոքային պաշարումը։ The disease may adversely impact the heart's electrical conduction system and can cause abnormal heart rhythms such as atrioventricular block.[31]
Late disseminated infection
[խմբագրել | խմբագրել կոդը]After several months, untreated or inadequately treated people may go on to develop severe and chronic symptoms that affect many parts of the body, including the brain, nerves, eyes, joints, and heart. Many disabling symptoms can occur, including permanent impairment of motor or sensory function of the lower extremities in extreme cases.[23] The associated nerve pain radiating out from the spine is termed Bannwarth syndrome,[32] named after Alfred Bannwarth.
The late disseminated stage is where the infection has fully spread throughout the body. Chronic neurologic symptoms occur in up to 5% of untreated people.[25] A polyneuropathy that involves shooting pains, numbness, and tingling in the hands or feet may develop. A neurologic syndrome called Lyme encephalopathy is associated with subtle cognitive difficulties, insomnia, a general sense of feeling unwell, and changes in personality.[33] Other problems, however, such as depression and fibromyalgia, are no more common in people with Lyme disease than in the general population.[34][35]
Chronic encephalomyelitis, which may be progressive, can involve cognitive impairment, brain fog, migraines, balance issues, weakness in the legs, awkward gait, facial palsy, bladder problems, vertigo, and back pain. In rare cases, untreated Lyme disease may cause frank psychosis, which has been misdiagnosed as schizophrenia or bipolar disorder. Panic attacks and anxiety can occur; also, delusional behavior may be seen, including somatoform delusions, sometimes accompanied by a depersonalization or derealization syndrome, where the patients begin to feel detached from themselves or from reality.[36][37]
A number of studies have found the causative agent of Lyme Borrelia burgdorferi in both the meninges and brains of people with neurological symptoms.[38]
Lyme arthritis usually affects the knees.[39] In a minority of people, arthritis can occur in other joints, including the ankles, elbows, wrists, hips, and shoulders. Pain is often mild or moderate, usually with swelling at the involved joint. Baker's cysts may form and rupture. In some cases, joint erosion occurs.
Acrodermatitis chronica atrophicans (ACA) is a chronic skin disorder observed primarily in Europe among the elderly.[28] ACA begins as a reddish-blue patch of discolored skin, often on the backs of the hands or feet. The lesion slowly atrophies over several weeks or months, with the skin becoming first thin and wrinkled and then, if untreated, completely dry and hairless.[40]
Cause
[խմբագրել | խմբագրել կոդը]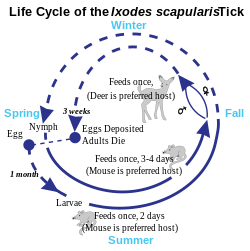



Lyme disease is caused by spirochetes, spiral bacteria from the genus Borrelia. Spirochetes are surrounded by peptidoglycan and flagella, along with an outer membrane similar to other Gram-negative bacteria. Because of their double-membrane envelope, Borrelia bacteria are often mistakenly described as Gram negative despite the considerable differences in their envelope components from Gram-negative bacteria.[41] The Lyme-related Borrelia species are collectively known as Borrelia burgdorferi sensu lato, and show a great deal of genetic diversity.
B. burgdorferi sensu lato is made up of 21 closely related species, but only three clearly cause Lyme disease: B. burgdorferi sensu stricto (predominant in North America, but also present in Europe), B. afzelii, and B. garinii (both predominant in Eurasia).[42][43] Some studies have also proposed B. bissettii and B. valaisiana may sometimes infect humans, but these species do not seem to be important causes of disease.[44][45]
Transmission
[խմբագրել | խմբագրել կոդը]Lyme disease is classified as a zoonosis, as it is transmitted to humans from a natural reservoir among small mammals and birds by ticks that feed on both sets of hosts.[46] Hard-bodied ticks of the genus Ixodes are the main vectors of Lyme disease (also the vector for Babesia).[47] Most infections are caused by ticks in the nymphal stage, because they are very small and thus may feed for long periods of time undetected.[46] In New Jersey, USA, nymphal ticks are generally the size of a poppy seed and sometimes with a dark head and a translucent body.[48] (The younger larval ticks are very rarely infected.[49]) Although deer are the preferred hosts of adult deer ticks, and tick populations are much lower in the absence of deer, ticks generally do not acquire Borrelia from deer, instead they obtain them from infected small mammals such as the white-footed mouse, and occasionally birds.[50]
Within the tick midgut, the Borrelia's outer surface protein A (OspA) binds to the tick receptor for OspA, known as TROSPA. When the tick feeds, the Borrelia downregulates OspA and upregulates OspC, another surface protein. After the bacteria migrate from the midgut to the salivary glands, OspC binds to Salp15, a tick salivary protein that appears to have immunosuppressive effects that enhance infection.[51] Successful infection of the mammalian host depends on bacterial expression of OspC.[52]
Tick bites often go unnoticed because of the small size of the tick in its nymphal stage, as well as tick secretions that prevent the host from feeling any itch or pain from the bite. However, transmission is quite rare, with only about 1% of recognized tick bites resulting in Lyme disease.
In Europe, the vector is Ixodes ricinus, which is also called the sheep tick or castor bean tick.[53] In China, Ixodes persulcatus (the taiga tick) is probably the most important vector.[54] In North America, the black-legged tick or deer tick (Ixodes scapularis) is the main vector on the East Coast.[49]
The lone star tick (Amblyomma americanum), which is found throughout the Southeastern United States as far west as Texas, is unlikely to transmit the Lyme disease spirochetes,[55] though it may be implicated in a related syndrome called southern tick-associated rash illness, which resembles a mild form of Lyme disease.[56]
On the West Coast of the United States, the main vector is the western black-legged tick (Ixodes pacificus).[57] The tendency of this tick species to feed predominantly on host species such as lizards that are resistant to Borrelia infection appears to diminish transmission of Lyme disease in the West.[58][59]
Transmission can occur across the placenta during pregnancy and as with a number of other spirochetal diseases, adverse pregnancy outcomes are possible with untreated infection; prompt treatment with antibiotics reduces or eliminates this risk.[60][61][62][63][64]
While Lyme spirochetes have been found in insects, as well as ticks,[65] reports of actual infectious transmission appear to be rare.[66] Lyme spirochete DNA has been found in semen[67] and breast milk.[68] However, according to the CDC, live spirochetes have not been found in breast milk, urine, or semen and thus is not sexually transmitted.[69]
Tick-borne coinfections
[խմբագրել | խմբագրել կոդը]Ticks that transmit B. burgdorferi to humans can also carry and transmit several other parasites, such as Theileria microti and Anaplasma phagocytophilum, which cause the diseases babesiosis and human granulocytic anaplasmosis (HGA), respectively.[70] Among early Lyme disease patients, depending on their location, 2–12% will also have HGA and 2–40% will have babesiosis.[71] Ticks in certain regions, including the lands along the eastern Baltic Sea, also transmit tick-borne encephalitis.[72]
Coinfections complicate Lyme symptoms, especially diagnosis and treatment. It is possible for a tick to carry and transmit one of the coinfections and not Borrelia, making diagnosis difficult and often elusive. The Centers for Disease Control and Prevention studied 100 ticks in rural New Jersey, and found 55% of the ticks were infected with at least one of the pathogens.[73]
Pathophysiology
[խմբագրել | խմբագրել կոդը]B. burgdorferi can spread throughout the body during the course of the disease, and has been found in the skin, heart, joints, peripheral nervous system, and central nervous system.[52][74] Many of the signs and symptoms of Lyme disease are a consequence of the immune response to the spirochete in those tissues.[25]
B. burgdorferi is injected into the skin by the bite of an infected Ixodes tick. Tick saliva, which accompanies the spirochete into the skin during the feeding process, contains substances that disrupt the immune response at the site of the bite.[75] This provides a protective environment where the spirochete can establish infection. The spirochetes multiply and migrate outward within the dermis. The host inflammatory response to the bacteria in the skin causes the characteristic circular EM lesion.[52] Neutrophils, however, which are necessary to eliminate the spirochetes from the skin, fail to appear in the developing EM lesion. This allows the bacteria to survive and eventually spread throughout the body.[76]
Days to weeks following the tick bite, the spirochetes spread via the bloodstream to joints, heart, nervous system, and distant skin sites, where their presence gives rise to the variety of symptoms of the disseminated disease. The spread of B. burgdorferi is aided by the attachment of the host protease plasmin to the surface of the spirochete.[77]
If untreated, the bacteria may persist in the body for months or even years, despite the production of B. burgdorferi antibodies by the immune system.[78] The spirochetes may avoid the immune response by decreasing expression of surface proteins that are targeted by antibodies, antigenic variation of the VlsE surface protein, inactivating key immune components such as complement, and hiding in the extracellular matrix, which may interfere with the function of immune factors.[79][80]
In the brain, B. burgdorferi may induce astrocytes to undergo astrogliosis (proliferation followed by apoptosis), which may contribute to neurodysfunction.[81] The spirochetes may also induce host cells to secrete quinolinic acid, which stimulates the NMDA receptor on nerve cells, which may account for the fatigue and malaise observed with Lyme encephalopathy.[82] In addition, diffuse white matter pathology during Lyme encephalopathy may disrupt gray matter connections, and could account for deficits in attention, memory, visuospatial ability, complex cognition, and emotional status. White matter disease may have a greater potential for recovery than gray matter disease, perhaps because the neuronal loss is less common. Resolution of MRI white matter hyperintensities after antibiotic treatment has been observed.[83]
Tryptophan, a precursor to serotonin, appears to be reduced within the central nervous system in a number of infectious diseases that affect the brain, including Lyme.[84] Researchers are investigating if this neurohormone secretion is the cause of neuropsychiatric disorders developing in some patients with borreliosis.[85]
Immunological studies
[խմբագրել | խմբագրել կոդը]Exposure to the Borrelia bacterium during Lyme disease possibly causes a long-lived and damaging inflammatory response,[86] a form of pathogen-induced autoimmune disease.[87] The production of this reaction might be due to a form of molecular mimicry, where Borrelia avoids being killed by the immune system by resembling normal parts of the body's tissues.[88][89]
Chronic symptoms from an autoimmune reaction could explain why some symptoms persist even after the spirochetes have been eliminated from the body. This hypothesis may explain why chronic arthritis persists after antibiotic therapy, similar to rheumatic fever, but its wider application is controversial.[90][91]
Diagnosis
[խմբագրել | խմբագրել կոդը]Lyme disease is diagnosed clinically based on symptoms, objective physical findings (such as EM, facial palsy, or arthritis), or a history of possible exposure to infected ticks, as well as serological blood tests. The EM rash is not always a bull's eye, i.e., it can be solid red. When making a diagnosis of Lyme disease, health care providers should consider other diseases that may cause similar illnesses. Not all individuals infected with Lyme disease develop the characteristic bull's-eye rash, and many may not recall a tick bite.[92]
Because of the difficulty in culturing Borrelia bacteria in the laboratory, diagnosis of Lyme disease is typically based on the clinical exam findings and a history of exposure to endemic Lyme areas.[47] The EM rash, which does not occur in all cases, is considered sufficient to establish a diagnosis of Lyme disease even when serologic blood tests are negative.[93][94] Serological testing can be used to support a clinically suspected case, but is not diagnostic by itself.[47]
Diagnosis of late-stage Lyme disease is often complicated by a multifaceted appearance and nonspecific symptoms, prompting one reviewer to call Lyme the new "great imitator".[95] Lyme disease may be misdiagnosed as multiple sclerosis, rheumatoid arthritis, fibromyalgia, chronic fatigue syndrome, lupus, Crohn's disease, HIV, or other autoimmune and neurodegenerative diseases. As all people with later-stage infection will have a positive antibody test, simple blood tests can exclude Lyme disease as a possible cause of a person's symptoms.[96]
Laboratory testing
[խմբագրել | խմբագրել կոդը]Several forms of laboratory testing for Lyme disease are available, some of which have not been adequately validated. The most widely used tests are serologies, which measure levels of specific antibodies in a patient's blood. These tests may be negative in early infection as the body may not have produced a significant quantity of antibodies, but they are considered a reliable aid in the diagnosis of later stages of Lyme disease.[97] Serologic tests for Lyme disease are of limited use in people lacking objective signs of Lyme disease because of false positive results and cost.[98]
The serological laboratory tests most widely available and employed are the Western blot and ELISA. A two-tiered protocol is recommended by the Centers for Disease Control and Prevention: the sensitive ELISA test is performed first, and if it is positive or equivocal, then the more specific Western blot is run.[99] The reliability of testing in diagnosis remains controversial.[47] Studies show the Western blot IgM has a specificity of 94–96% for people with clinical symptoms of early Lyme disease.[100][101] The initial ELISA test has a sensitivity of about 70%, and in two-tiered testing, the overall sensitivity is only 64%, although this rises to 100% in the subset of people with disseminated symptoms, such as arthritis.[102]
Erroneous test results have been widely reported in both early and late stages of the disease, and can be caused by several factors, including antibody cross-reactions from other infections, including Epstein–Barr virus and cytomegalovirus,[103] as well as herpes simplex virus.[104] The overall rate of false positives is low, only about 1 to 3%, in comparison to a false-negative rate of up to 36% in the early stages of infection using two-tiered testing.[102]
Polymerase chain reaction (PCR) tests for Lyme disease have also been developed to detect the genetic material (DNA) of the Lyme disease spirochete. PCR tests are susceptible to false positive results from poor laboratory technique.[105] Even when properly performed, PCR often shows false negative results with blood and cerebrospinal fluid specimens.[106] Hence, PCR is not widely performed for diagnosis of Lyme disease, but it may have a role in the diagnosis of Lyme arthritis because it is a highly sensitive way of detecting ospA DNA in synovial fluid.[107]
Culture or PCR are the current means for detecting the presence of the organism, as serologic studies only test for antibodies of Borrelia. OspA antigens, shed by live Borrelia bacteria into urine, are a promising technique being studied.[108] The use of nanotrap particles for their detection is being looked at and the OspA has been linked to active symptoms of Lyme.[109][110] High titers of either immunoglobulin G (IgG) or immunoglobulin M (IgM) antibodies to Borrelia antigens indicate disease, but lower titers can be misleading, because the IgM antibodies may remain after the initial infection, and IgG antibodies may remain for years.[111]
Western blot, ELISA, and PCR can be performed by either blood test via venipuncture or cerebrospinal fluid (CSF) via lumbar puncture. Though lumbar puncture is more definitive of diagnosis, antigen capture in the CSF is much more elusive; reportedly, CSF yields positive results in only 10–30% of affected individuals cultured. The diagnosis of neurologic infection by Borrelia should not be excluded solely on the basis of normal routine CSF or negative CSF antibody analyses.[112]
New techniques for clinical testing of Borrelia infection have been developed, such as LTT-MELISA,[113] although the results of studies are contradictory. The first peer reviewed study assessing the diagnostic sensitivity and specificity of the test was presented in 2012 and demonstrated potential for LTT to become a supportive diagnostic tool.[114] In 2014, research of LTT-MELISA concluded that it is "sensible" to include the LTT test in the diagnostic protocol for putative European-acquired Lyme borreliosis infections.[115] Other diagnostic techniques, such as focus floating microscopy, are under investigation.[116] New research indicates chemokine CXCL13 may also be a possible marker for neuroborreliosis.[117]
Some laboratories offer Lyme disease testing using assays whose accuracy and clinical usefulness have not been adequately established. These tests include urine antigen tests, PCR tests on urine, immunofluorescent staining for cell-wall-deficient forms of B. burgdorferi, and lymphocyte transformation tests. The CDC does not recommend these tests, and stated their use is "of great concern and is strongly discouraged".[106]
Imaging
[խմբագրել | խմբագրել կոդը]Neuroimaging is controversial in whether it provides specific patterns unique to neuroborreliosis, but may aid in differential diagnosis and in understanding the pathophysiology of the disease.[118] Though controversial, some evidence shows certain neuroimaging tests can provide data that are helpful in the diagnosis of a patient. Magnetic resonance imaging (MRI) and single-photon emission computed tomography (SPECT) are two of the tests that can identify abnormalities in the brain of a patient affected with this disease. Neuroimaging findings in an MRI include lesions in the periventricular white matter, as well as enlarged ventricles and cortical atrophy. The findings are considered somewhat unexceptional because the lesions have been found to be reversible following antibiotic treatment. Images produced using SPECT show numerous areas where an insufficient amount of blood is being delivered to the cortex and subcortical white matter. However, SPECT images are known to be nonspecific because they show a heterogeneous pattern in the imaging. The abnormalities seen in the SPECT images are very similar to those seen in people with cerebral vacuities and Creutzfeldt–Jakob disease, which makes them questionable.[119]
Prevention
[խմբագրել | խմբագրել կոդը]Protective clothing includes a hat, long-sleeved shirt, and long pants tucked into socks or boots. Light-colored clothing makes the tick more easily visible before it attaches itself. People should use special care in handling and allowing outdoor pets inside homes because they can bring ticks into the house. People who work in areas with woods, bushes, leaf litter, and tall grass are at risk of becoming infected with Lyme at work. Employers can reduce the risk for employees by providing education on Lyme transmission and infection risks, and about how to check themselves for ticks on the groin, armpits, and hair. Work clothing used in risky areas should be washed in hot water and dried in a hot dryer to kill any ticks.[120]
Permethrin sprayed on clothing kills ticks on contact, and is sold for this purpose. According to the CDC, only DEET is effective at repelling ticks.[121]
Host animals
[խմբագրել | խմբագրել կոդը]Lyme and other deer tick-borne diseases can sometimes be reduced by greatly reducing the deer population on which the adult ticks depend for feeding and reproduction. Lyme disease cases fell following deer eradication on an island, Monhegan, Maine[122] and following deer control in Mumford Cove, Connecticut.[123] It is worth noting that eliminating deer may lead to a temporary increase in tick density.[124]
For example, in the U.S., reducing the deer population to levels of 8 to 10 per square mile (from the current levels of 60 or more deer per square mile in the areas of the country with the highest Lyme disease rates), may reduce tick numbers and reduce the spread of Lyme and other tick-borne diseases.[125] However, such a drastic reduction may be very difficult to implement in many areas, and low to moderate densities of deer or other large mammal hosts may continue to feed sufficient adult ticks to maintain larval densities at high levels. Routine veterinary control of ticks of domestic animals, including livestock, by use of acaricides can contribute to reducing exposure of humans to ticks.
Action can be taken to avoid getting bitten by ticks by using insect repellants, for example, those that contain DEET. DEET-containing repellants are thought to be moderately effective in the prevention of tick bites.[126]
In Europe known reservoirs of Borrelia burgdorferi were 9 small mammals, 7 medium-sized mammals and 16 species of birds (including passerines, sea-birds and pheasants).[127] These animals seem to transmit spirochetes to ticks and thus participate in the natural circulation of B. burgdorferi in Europe. The house mouse is also suspected as well as other species of small rodents, particularly in Eastern Europe and Russia.[127]
"The reservoir species that contain the most pathogens are the European roe deer Capreolus capreolus;[128] "it does not appear to serve as a major reservoir of B. burgdorferi" thought Jaenson & al. (1992)[129] (incompetent host for B. burgdorferi and TBE virus) but it is important for feeding the ticks,[130] as red deer and wild boars (Sus scrofa),[131] in which one Rickettsia and three Borrelia species were identified",[128] with high risks of coinfection in roe deer.[132] Nevertheless, in the 2000s, in roe deer in Europe " two species of Rickettsia and two species of Borrelia were identified".[131]
Vaccination
[խմբագրել | խմբագրել կոդը]A recombinant vaccine against Lyme disease, based on the outer surface protein A (ospA) of B. burgdorferi, was developed by SmithKline Beecham. In clinical trials involving more than 10,000 people, the vaccine, called LYMErix, was found to confer protective immunity to Borrelia in 76% of adults and 100% of children with only mild or moderate and transient adverse effects.[133] LYMErix was approved on the basis of these trials by the Food and Drug Administration (FDA) on 21 December 1998.
Following approval of the vaccine, its entry in clinical practice was slow for a variety of reasons, including its cost, which was often not reimbursed by insurance companies.[134] Subsequently, hundreds of vaccine recipients reported they had developed autoimmune and other side effects. Supported by some patient advocacy groups, a number of class-action lawsuits were filed against GlaxoSmithKline, alleging the vaccine had caused these health problems. These claims were investigated by the FDA and the Centers for Disease Control, which found no connection between the vaccine and the autoimmune complaints.[135]
Despite the lack of evidence that the complaints were caused by the vaccine, sales plummeted and LYMErix was withdrawn from the U.S. market by GlaxoSmithKline in February 2002,[136] in the setting of negative media coverage and fears of vaccine side effects.[135][137] The fate of LYMErix was described in the medical literature as a "cautionary tale";[137] an editorial in Nature cited the withdrawal of LYMErix as an instance in which "unfounded public fears place pressures on vaccine developers that go beyond reasonable safety considerations."[19] The original developer of the OspA vaccine at the Max Planck Institute told Nature: "This just shows how irrational the world can be... There was no scientific justification for the first OspA vaccine LYMErix being pulled."[135]
Vaccines have been formulated and approved for prevention of Lyme disease in dogs. Currently, three Lyme disease vaccines are available. LymeVax, formulated by Fort Dodge Laboratories, contains intact dead spirochetes which expose the host to the organism. Galaxy Lyme, Intervet-Schering-Plough's vaccine, targets proteins OspC and OspA. The OspC antibodies kill any of the bacteria that have not been killed by the OspA antibodies. Canine Recombinant Lyme, formulated by Merial, generates antibodies against the OspA protein so a tick feeding on a vaccinated dog draws in blood full of anti-OspA antibodies, which kill the spirochetes in the tick's gut before they are transmitted to the dog.[138]
Valneva's hexavalent (OspA) protein subunit-based vaccine candidate VLA15 was granted fast track designation by the U.S. Food and Drug Administration in July 2017 which will allow further study.[139]
Tick removal
[խմբագրել | խմբագրել կոդը]
Attached ticks should be removed promptly, as removal within 36 hours can reduce transmission rates.[140] Folk remedies for tick removal tend to be ineffective, offer no advantages in preventing the transfer of disease, and may increase the risks of transmission or infection.[141] The best method is simply to pull the tick out with tweezers as close to the skin as possible, without twisting, and avoiding crushing the body of the tick or removing the head from the tick's body.[142] The risk of infection increases with the time the tick is attached, and if a tick is attached for less than 24 hours, infection is unlikely. However, since these ticks are very small, especially in the nymph stage, prompt detection is quite difficult.[140] The Australasian Society of Clinical Immunology and Allergy does not recommend the use of tweezers where the person may be allergic as anaphylaxis could result. Instead they recommend killing the tick first by using a product to rapidly freeze the tick to prevent it from injecting more allergen-containing saliva and the tick should then be removed in a safe place such as a hospital emergency room.[143]
Preventive antibiotics
[խմբագրել | խմբագրել կոդը]The risk of infectious transmission increases with the duration of tick attachment.[144] It requires between 36 and 48 hours of attachment for the bacteria that causes Lyme to travel from within the tick into its saliva.[144] If a deer tick that is sufficiently likely to be carrying Borrelia is found attached to a person and removed, and if the tick has been attached for 36 hours or is engorged, a single dose of doxycycline administered within the 72 hours after removal may reduce the risk of Lyme disease. It is not generally recommended for all people bitten, as development of infection is rare: about 50 bitten people would have to be treated this way to prevent one case of erythema migrans (i.e. the typical rash found in about 70-80% of people infected).[1][144]
Occupational exposure
[խմբագրել | խմբագրել կոդը]Outdoor workers are at risk of Lyme disease if they work at sites with infected ticks. In 2010, the highest number of confirmed Lyme disease cases were reported from New Jersey, Pennsylvania, Wisconsin, New York, Massachusetts, Connecticut, Minnesota, Maryland, Virginia, New Hampshire, Delaware, and Maine. U.S. workers in the northeastern and north-central States are at highest risk of exposure to infected ticks. Ticks may also transmit other tick-borne diseases to workers in these and other regions of the country. Worksites with woods, bushes, high grass, or leaf litter are likely to have more ticks. Outdoor workers should be most careful to protect themselves in the late spring and summer when young ticks are most active.[145]
Treatment
[խմբագրել | խմբագրել կոդը]Antibiotics are the primary treatment.[1][144] The specific approach to their use is dependent on the individual affected and the stage of the disease.[144] For most people with early localized infection, oral administration of doxycycline is widely recommended as the first choice, as it is effective against not only Borrelia bacteria but also a variety of other illnesses carried by ticks.[144] Doxycycline is contraindicated in children younger than eight years of age and women who are pregnant or breastfeeding;[144] alternatives to doxycycline are amoxicillin, cefuroxime axetil, and azithromycin.[144] Individuals with early disseminated or late infection may have symptomatic cardiac disease, refractory Lyme arthritis, or neurologic symptoms like meningitis or encephalitis.[144] Intravenous administration of ceftriaxone is recommended as the first choice in these cases;[144] cefotaxime and doxycycline are available as alternatives.[144]
These treatment regimens last from one to four weeks.[144] If joint swelling persists or returns, a second round of antibiotics may be considered.[144] Outside of that, a prolonged antibiotic regimen lasting more than 28 days is not recommended as no clinical evidence shows it to be effective.[144][146] IgM and IgG antibody levels may be elevated for years even after successful treatment with antibiotics.[144] As antibody levels are not indicative of treatment success, testing for them is not recommended.[144]
Prognosis
[խմբագրել | խմբագրել կոդը]For early cases, promptԿաղապար:Specify treatment is usually curative.[147] However, the severity and treatment of Lyme disease may be complicated due to late diagnosis, failure of antibiotic treatment, and simultaneous infection with other tick-borne diseases (coinfections), including ehrlichiosis, babesiosis, and immune suppression[փա՞ստ] in the patient.
It is believed that less than 5% of people have lingering symptoms of fatigue, pain, or joint and muscle aches at the time they finish treatment.[148] These symptoms can last for more than 6 months. This condition is called post-treatment lyme disease syndrome. As of 2016 the reason for the lingering symptoms was not known; the condition is generally managed similarly to fibromyalgia or chronic fatigue syndrome.[149]
In dogs, a serious long-term prognosis may result in glomerular disease,[150] which is a category of kidney damage that may cause chronic kidney disease.[138] Dogs may also experience chronic joint disease if the disease is left untreated. However, the majority of cases of Lyme disease in dogs result in a complete recovery with, and sometimes without, treatment with antibiotics.[151]Կաղապար:Verify source In rare cases, Lyme disease can be fatal to both humans and dogs.[152]
Epidemiology
[խմբագրել | խմբագրել կոդը]
Lyme disease occurs regularly in Northern Hemisphere temperate regions.[153]
Africa
[խմբագրել | խմբագրել կոդը]In northern Africa, B. burgdorferi sensu lato has been identified in Morocco, Algeria, Egypt and Tunisia.[154][155][156]
Lyme disease in sub-Saharan Africa is presently unknown, but evidence indicates it may occur in humans in this region. The abundance of hosts and tick vectors would favor the establishment of Lyme infection in Africa.[157] In East Africa, two cases of Lyme disease have been reported in Kenya.[158]
Asia
[խմբագրել | խմբագրել կոդը]B. burgdorferi sensu lato-infested ticks are being found more frequently in Japan, as well as in northwest China, Nepal, Thailand and far eastern Russia.[159][160] Borrelia has also been isolated in Mongolia.[161]
Europe
[խմբագրել | խմբագրել կոդը]In Europe, Lyme disease is caused by infection with one or more pathogenic European genospecies of the spirochaete B. burgdorferi sensu lato, mainly transmitted by the tick Ixodes ricinus.[162] Cases of B. burgdorferi sensu lato-infected ticks are found predominantly in central Europe, particularly in Slovenia and Austria, but have been isolated in almost every country on the continent.[163] Incidence in southern Europe, such as Italy and Portugal, is much lower.[164]
United Kingdom
[խմբագրել | խմբագրել կոդը]In the United Kingdom the number of laboratory confirmed cases of Lyme disease has been rising steadily since voluntary reporting was introduced in 1986[165] when 68 cases were recorded in the UK and Republic of Ireland combined.[166] In the UK there were 23 confirmed cases in 1988 and 19 in 1990,[167] but 973 in 2009[165] and 953 in 2010.[168] Provisional figures for the first 3 quarters of 2011 show a 26% increase on the same period in 2010.[169]
It is thought, however, that the actual number of cases is significantly higher than suggested by the above figures, with the UK's Health Protection Agency estimating that there are between 2,000 and 3,000 cases per year,[168] (with an average of around 15% of the infections acquired overseas[165]), while Dr Darrel Ho-Yen, Director of the Scottish Toxoplasma Reference Laboratory and National Lyme Disease Testing Service, believes that the number of confirmed cases should be multiplied by 10 "to take account of wrongly diagnosed cases, tests giving false results, sufferers who weren't tested, people who are infected but not showing symptoms, failures to notify and infected individuals who don't consult a doctor."[170][171]
Despite Lyme disease (Borrelia burgdorferi infection) being a notifiable disease in Scotland[172] since January 1990[173] which should therefore be reported on the basis of clinical suspicion, it is believed that many GPs are unaware of the requirement.[174] Mandatory reporting, limited to laboratory test results only, was introduced throughout the UK in October 2010, under the Health Protection (Notification) Regulations 2010.[165]
Although there is a greater incidence of Lyme disease in the New Forest, Salisbury Plain, Exmoor, the South Downs, parts of Wiltshire and Berkshire, Thetford Forest[175] and the West coast and islands of Scotland[176] infected ticks are widespread, and can even be found in the parks of London.[167][177] A 1989 report found that 25% of forestry workers in the New Forest were seropositive, as were between 2% and 4-5% of the general local population of the area.[178][179]
Tests on pet dogs, carried out throughout the country in 2009 indicated that around 2.5% of ticks in the UK may be infected, considerably higher than previously thought.[180][181] It is thought that global warming may lead to an increase in tick activity in the future, as well as an increase in the amount of time that people spend in public parks, thus increasing the risk of infection.[182]
North America
[խմբագրել | խմբագրել կոդը]Many studies in North America have examined ecological and environmental correlates of Lyme disease prevalence. A 2005 study using climate suitability modelling of I. scapularis projected that climate change would cause an overall 213% increase in suitable vector habitat by the year 2080, with northward expansions in Canada, increased suitability in the central U.S., and decreased suitable habitat and vector retraction in the southern U.S.[183] A 2008 review of published studies concluded that the presence of forests or forested areas was the only variable that consistently elevated the risk of Lyme disease whereas other environmental variables showed little or no concordance between studies.[184] The authors argued that the factors influencing tick density and human risk between sites are still poorly understood, and that future studies should be conducted over longer time periods, become more standardized across regions, and incorporate existing knowledge of regional Lyme disease ecology.[184]
Canada
[խմբագրել | խմբագրել կոդը]Owing to changing climate, the range of ticks able to carry Lyme disease has expanded from a limited area of Ontario to include areas of southern Quebec, Manitoba, northern Ontario, southern New Brunswick, southwest Nova Scotia and limited parts of Saskatchewan and Alberta, as well as British Columbia. Cases have been reported as far east as the island of Newfoundland.[185][186][187] A model-based prediction by Leighton et al. (2012) suggests that the range of the I. scapularis tick will expand into Canada by 46 km/year over the next decade, with warming climatic temperatures as the main driver of increased speed of spread.[188]
Mexico
[խմբագրել | խմբագրել կոդը]A 2007 study suggests Borrelia burgdorferi infections are endemic to Mexico, from four cases reported between 1999 and 2000.[189]
United States
[խմբագրել | խմբագրել կոդը]
Each year, approximately 30,000 new cases are reported to the CDC however, this number is likely underestimated. The CDC is currently conducting research on evaluation and diagnostics of the disease and preliminary results suggest the number of new cases to be around 300,000.[190][191]
Lyme disease is the most common tick-borne disease in North America and Europe, and one of the fastest-growing infectious diseases in the United States. Of cases reported to the United States CDC, the ratio of Lyme disease infection is 7.9 cases for every 100,000 persons. In the ten states where Lyme disease is most common, the average was 31.6 cases for every 100,000 persons for the year 2005.[192][193][194]
Although Lyme disease has been reported in all states[190][195] about 99% of all reported cases are confined to just five geographic areas (New England, Mid-Atlantic, East-North Central, South Atlantic, and West North-Central).[196] New 2011 CDC Lyme case definition guidelines are used to determine confirmed CDC surveillance cases.[197]
Effective January 2008, the CDC gives equal weight to laboratory evidence from 1) a positive culture for B. burgdorferi; 2) two-tier testing (ELISA screening and Western blot confirming); or 3) single-tier IgG (old infection) Western blot.[198] Previously, the CDC only included laboratory evidence based on (1) and (2) in their surveillance case definition. The case definition now includes the use of Western blot without prior ELISA screen.[198]
The number of reported cases of the disease has been increasing, as are endemic regions in North America. For example, B. burgdorferi sensu lato was previously thought to be hindered in its ability to be maintained in an enzootic cycle in California, because it was assumed the large lizard population would dilute the prevalence of B. burgdorferi in local tick populations; this has since been brought into question, as some evidence has suggested lizards can become infected.[199]
Except for one study in Europe,[200] much of the data implicating lizards is based on DNA detection of the spirochete and has not demonstrated that lizards are able to infect ticks feeding upon them.[199][201][202][203] As some experiments suggest lizards are refractory to infection with Borrelia, it appears likely their involvement in the enzootic cycle is more complex and species-specific.[59]
While B. burgdorferi is most associated with ticks hosted by white-tailed deer and white-footed mice, Borrelia afzelii is most frequently detected in rodent-feeding vector ticks, and Borrelia garinii and Borrelia valaisiana appear to be associated with birds. Both rodents and birds are competent reservoir hosts for B. burgdorferi sensu stricto. The resistance of a genospecies of Lyme disease spirochetes to the bacteriolytic activities of the alternative complement pathway of various host species may determine its reservoir host association.[փա՞ստ]
Several similar but apparently distinct conditions may exist, caused by various species or subspecies of Borrelia in North America. A regionally restricted condition that may be related to Borrelia infection is southern tick-associated rash illness (STARI), also known as Masters' disease. Amblyomma americanum, known commonly as the lone-star tick, is recognized as the primary vector for STARI. In some parts of the geographical distribution of STARI, Lyme disease is quite rare (e.g., Arkansas), so patients in these regions experiencing Lyme-like symptoms—especially if they follow a bite from a lone-star tick—should consider STARI as a possibility. It is generally a milder condition than Lyme and typically responds well to antibiotic treatment.[փա՞ստ]
In recent years there have been 5 to 10 cases a year of a disease similar to Lyme occurring in Montana. It occurs primarily in pockets along the Yellowstone River in central Montana. People have developed a red bull's-eye rash around a tick bite followed by weeks of fatigue and a fever.[195]
Lyme disease prevalence is comparable among males and females. A wide range of age groups is affected, though the number of cases is highest among 10- to 19-year-olds. For unknown reasons, Lyme disease is seven times more common among Asians.[204]
South America
[խմբագրել | խմբագրել կոդը]In South America, tick-borne disease recognition and occurrence is rising. In Brazil, a Lyme-like disease known as Baggio–Yoshinari syndrome was identified, caused by microorganisms that do not belong to the B. burgdorferi sensu lato complex and transmitted by ticks of the Amblyomma and Rhipicephalus genera.[205] The first reported case of BYS in Brazil was made in 1992 in Cotia, São Paulo.[206] B. burgdorferi sensu stricto antigens in patients have been identified in Colombia and Bolivia.[փա՞ստ]
History
[խմբագրել | խմբագրել կոդը]The evolutionary history of Borrelia burgdorferi genetics has been the subject of recent studies. One study has found that prior to the reforestation that accompanied post-colonial farm abandonment in New England and the wholesale migration into the mid-west that occurred during the early 19th century, Lyme disease was present for thousands of years in America and had spread along with its tick hosts from the Northeast to the Midwest.[207]
John Josselyn, who visited New England in 1638 and again from 1663–1670, wrote "there be infinite numbers of tikes hanging upon the bushes in summer time that will cleave to man's garments and creep into his breeches eating themselves in a short time into the very flesh of a man. I have seen the stockins of those that have gone through the woods covered with them."[208]
This is also confirmed by the writings of Peter Kalm, a Swedish botanist who was sent to America by Linnaeus, and who found the forests of New York "abound" with ticks when he visited in 1749. When Kalm's journey was retraced 100 years later, the forests were gone and the Lyme bacterium had probably become isolated to a few pockets along the northeast coast, Wisconsin, and Minnesota.[209]
Perhaps the first detailed description of what is now known as Lyme disease appeared in the writings of Reverend Dr. John Walker after a visit to the Island of Jura (Deer Island) off the west coast of Scotland in 1764.[210] He gives a good description both of the symptoms of Lyme disease (with "exquisite pain [in] the interior parts of the limbs") and of the tick vector itself, which he describes as a "worm" with a body which is "of a reddish colour and of a compressed shape with a row of feet on each side" that "penetrates the skin". Many people from this area of Great Britain emigrated to North America between 1717 and the end of the 18th century.
The examination of preserved museum specimens has found Borrelia DNA in an infected Ixodes ricinus tick from Germany that dates back to 1884, and from an infected mouse from Cape Cod that died in 1894.[209] The 2010 autopsy of Ötzi the Iceman, a 5,300-year-old mummy, revealed the presence of the DNA sequence of Borrelia burgdorferi making him the earliest known human with Lyme disease.[211]
The early European studies of what is now known as Lyme disease described its skin manifestations. The first study dates to 1883 in Breslau, Germany (now Wrocław, Poland), where physician Alfred Buchwald described a man who had suffered for 16 years with a degenerative skin disorder now known as acrodermatitis chronica atrophicans.[212]
At a 1909 research conference, Swedish dermatologist Arvid Afzelius presented a study about an expanding, ring-like lesion he had observed in an older woman following the bite of a sheep tick. He named the lesion erythema migrans.[212] The skin condition now known as borrelial lymphocytoma was first described in 1911.[213]
The modern history of medical understanding of the disease, including its cause, diagnosis, and treatment, has been difficult.[214]
Neurological problems following tick bites were recognized starting in the 1920s. French physicians Garin and Bujadoux described a farmer with a painful sensory radiculitis accompanied by mild meningitis following a tick bite. A large, ring-shaped rash was also noted, although the doctors did not relate it to the meningoradiculitis. In 1930, the Swedish dermatologist Sven Hellerström was the first to propose EM and neurological symptoms following a tick bite were related.[215] In the 1940s, German neurologist Alfred Bannwarth described several cases of chronic lymphocytic meningitis and polyradiculoneuritis, some of which were accompanied by erythematous skin lesions.
Carl Lennhoff, who worked at the Karolinska Institute in Sweden, believed many skin conditions were caused by spirochetes. In 1948, he used a special stain to microscopically observe what he believed were spirochetes in various types of skin lesions, including EM.[216] Although his conclusions were later shown to be erroneous, interest in the study of spirochetes was sparked. In 1949, Nils Thyresson, who also worked at the Karolinska Institute, was the first to treat ACA with penicillin.[217] In the 1950s, the relationship among tick bite, lymphocytoma, EM and Bannwarth's syndrome was recognized throughout Europe leading to the widespread use of penicillin for treatment in Europe.[218][219]
In 1970, a dermatologist in Wisconsin named Rudolph Scrimenti recognized an EM lesion in a patient after recalling a paper by Hellerström that had been reprinted in an American science journal in 1950. This was the first documented case of EM in the United States. Based on the European literature, he treated the patient with penicillin.[220]
The full syndrome now known as Lyme disease was not recognized until a cluster of cases originally thought to be juvenile rheumatoid arthritis was identified in three towns in southeastern Connecticut in 1975, including the towns Lyme and Old Lyme, which gave the disease its popular name.[221] This was investigated by physicians David Snydman and Allen Steere of the Epidemic Intelligence Service, and by others from Yale University, including Dr. Stephen Malawista, who is credited as a co-discover of the disease.[222] The recognition that the patients in the United States had EM led to the recognition that "Lyme arthritis" was one manifestation of the same tick-borne condition known in Europe.[223]
Before 1976, the elements of B. burgdorferi sensu lato infection were called or known as tick-borne meningopolyneuritis, Garin-Bujadoux syndrome, Bannwarth syndrome, Afzelius' disease,[224] Montauk Knee or sheep tick fever. Since 1976 the disease is most often referred to as Lyme disease,[225][226] Lyme borreliosis or simply borreliosis.[փա՞ստ]
In 1980, Steere, et al., began to test antibiotic regimens in adult patients with Lyme disease.[227] In the same year, New York State Health Dept. epidemiologist Jorge Benach provided Willy Burgdorfer, a researcher at the Rocky Mountain Biological Laboratory, with collections of I. dammini [scapularis] from Shelter Island, NY, a known Lyme-endemic area as part of an ongoing investigation of Rocky Mountain spotted fever. In examining the ticks for rickettsiae, Burgdorfer noticed "poorly stained, rather long, irregularly coiled spirochetes." Further examination revealed spirochetes in 60% of the ticks. Burgdorfer credited his familiarity with the European literature for his realization that the spirochetes might be the "long-sought cause of ECM and Lyme disease." Benach supplied him with more ticks from Shelter Island and sera from patients diagnosed with Lyme disease. University of Texas Health Science Center researcher Alan Barbour "offered his expertise to culture and immunochemically characterize the organism." Burgdorfer subsequently confirmed his discovery by isolating, from patients with Lyme disease, spirochetes identical to those found in ticks.[228] In June 1982, he published his findings in Science, and the spirochete was named Borrelia burgdorferi in his honor.[229]
After the identification of B. burgdorferi as the causative agent of Lyme disease, antibiotics were selected for testing, guided by in vitro antibiotic sensitivities, including tetracycline antibiotics, amoxicillin, cefuroxime axetil, intravenous and intramuscular penicillin and intravenous ceftriaxone.[230][231] The mechanism of tick transmission was also the subject of much discussion. B. burgdorferi spirochetes were identified in tick saliva in 1987, confirming the hypothesis that transmission occurred via tick salivary glands.[232]
Society and culture
[խմբագրել | խմբագրել կոդը]Urbanization and other anthropogenic factors can be implicated in the spread of Lyme disease to humans. In many areas, expansion of suburban neighborhoods has led to gradual deforestation of surrounding wooded areas and increased border contact between humans and tick-dense areas. Human expansion has also resulted in a reduction of predators that hunt deer as well as mice, chipmunks and other small rodents—the primary reservoirs for Lyme disease. As a consequence of increased human contact with host and vector, the likelihood of transmission of the disease has greatly increased.[233][234] Researchers are investigating possible links between global warming and the spread of vector-borne diseases, including Lyme disease.[235]
Controversy
[խմբագրել | խմբագրել կոդը]The term "chronic Lyme disease" is controversial and not recognized in the medical literature,[236] and most medical authorities advise against long-term antibiotic treatment for Lyme disease.[98][237][238] Studies have shown that most people diagnosed with "chronic Lyme disease" either have no objective evidence of previous or current infection with B. burgdorferi or are people who should be classified as having post-treatment Lyme disease syndrome (PTLDS), which is defined as continuing or relapsing non-specific symptoms (such as fatigue, musculoskeletal pain, and cognitive complaints) in a person previously treated for Lyme disease.[239]
Other animals
[խմբագրել | խմբագրել կոդը]Prevention of Lyme disease is an important step in keeping dogs safe in endemic areas. Prevention education and a number of preventative measures are available. First, for dog owners who live near or who often frequent tick-infested areas, routine vaccinations of their dogs is an important step.[240]
Another crucial preventive measure is the use of persistent acaricides, such as topical repellents or pesticides that contain triazapentadienes (Amitraz), phenylpyrazoles (Fipronil), or permethrin (pyrethroids).[241] These acaricides target primarily the adult stages of Lyme-carrying ticks and reduce the number of reproductively active ticks in the environment.[240] Formulations of these ingredients are available in a variety of topical forms, including spot-ons, sprays, powders, impregnated collars, solutions, and shampoos.[241]
Examination of a dog for ticks after being in a tick-infested area is an important precautionary measure to take in the prevention of Lyme disease. Key spots to examine include the head, neck, and ears.[242]
Research
[խմբագրել | խմբագրել կոդը]The National Institutes of Health have supported research into bacterial persistence.[243]
References
[խմբագրել | խմբագրել կոդը]- ↑ 1,00 1,01 1,02 1,03 1,04 1,05 1,06 1,07 1,08 1,09 1,10 1,11 1,12 1,13 1,14 1,15 1,16 1,17 1,18 Shapiro ED (May 2014). «Clinical practice. Lyme disease» (PDF). The New England Journal of Medicine. 370 (18): 1724–31. doi:10.1056/NEJMcp1314325. PMC 4487875. PMID 24785207. Արխիվացված է օրիգինալից (PDF) 19 October 2016-ին.
- ↑ 2,00 2,01 2,02 2,03 2,04 2,05 2,06 2,07 2,08 2,09 «Signs and Symptoms of Lyme Disease». cdc.gov. 11 January 2013. Արխիվացված է օրիգինալից 16 January 2013-ին. Վերցված է 2 March 2015-ին.
- ↑ Aucott JN (June 2015). «Posttreatment Lyme disease syndrome». Infectious Disease Clinics of North America. 29 (2): 309–23. doi:10.1016/j.idc.2015.02.012. PMID 25999226.
- ↑ Johnson RC (1996). «Borrelia». In Baron S, և այլք: (eds.). Baron's Medical Microbiology (4th ed.). Univ of Texas Medical Branch. ISBN 978-0-9631172-1-2. PMID 21413339. Արխիվացված է օրիգինալից 7 February 2009-ին.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ 5,0 5,1 «Lyme disease transmission». cdc.gov. 11 January 2013. Արխիվացված է օրիգինալից 3 March 2015-ին. Վերցված է 2 March 2015-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ 6,0 6,1 Steere, AC; Strle, F; Wormser, GP; Hu, LT; Branda, JA; Hovius, JW; Li, X; Mead, PS (15 December 2016). «Lyme borreliosis». Nature Reviews. Disease Primers. 2: 16090. doi:10.1038/nrdp.2016.90. PMC 5539539. PMID 27976670.
- ↑ «Lyme borreliosis» (PDF). ECDC. Վերցված է 29 September 2018-ին.
- ↑ Pritt BS, Mead PS, Johnson DK, Neitzel DF, Respicio-Kingry LB, Davis JP, Schiffman E, Sloan LM, Schriefer ME, Replogle AJ, Paskewitz SM, Ray JA, Bjork J, Steward CR, Deedon A, Lee X, Kingry LC, Miller TK, Feist MA, Theel ES, Patel R, Irish CL, Petersen JM (May 2016). «Identification of a novel pathogenic Borrelia species causing Lyme borreliosis with unusually high spirochaetaemia: a descriptive study». The Lancet. Infectious Diseases. 16 (5): 556–564. doi:10.1016/S1473-3099(15)00464-8. PMC 4975683. PMID 26856777.
- ↑ «Lyme Disease Diagnosis and Testing». cdc.gov. 10 January 2013. Արխիվացված է օրիգինալից 2 March 2015-ին. Վերցված է 2 March 2015-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ «Two-step Laboratory Testing Process». cdc.gov. 15 November 2011. Արխիվացված է օրիգինալից 12 March 2015-ին. Վերցված է 2 March 2015-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ «Testing of Ticks». cdc.gov. 4 June 2013. Արխիվացված է օրիգինալից 19 February 2015-ին. Վերցված է 2 March 2015-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ «Tick Removal». cdc.gov. 23 June 2014. Արխիվացված է օրիգինալից 10 March 2015-ին. Վերցված է 2 March 2015-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ 13,0 13,1 13,2 «Post-Treatment Lyme Disease Syndrome». cdc.gov. 1 December 2017. Վերցված է 20 June 2018-ին.
- ↑ Regional Disease Vector Ecology Profile: Central Europe. DIANE Publishing. April 2001. էջ 136. ISBN 9781428911437. Արխիվացված է օրիգինալից 8 September 2017-ին.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Berger, Stephen (2014). Lyme disease: Global Status 2014 Edition. GIDEON Informatics Inc. էջ 7. ISBN 9781498803434. Արխիվացված է օրիգինալից 8 September 2017-ին.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ 16,0 16,1 Williams, Carolyn (2007). Infectious disease epidemiology : theory and practice (2nd ed.). Sudbury, Mass.: Jones and Bartlett Publishers. էջ 447. ISBN 9780763728793. Արխիվացված է օրիգինալից 8 September 2017-ին.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ «Willy Burgdorfer - obituary». Daily Telegraph. 1 December 2014. Արխիվացված է օրիգինալից 1 December 2014-ին. Վերցված է 1 December 2014-ին.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Lantos PM (June 2015). «Chronic Lyme disease». Infectious Disease Clinics of North America. 29 (2): 325–40. doi:10.1016/j.idc.2015.02.006. PMC 4477530. PMID 25999227.
- ↑ 19,0 19,1 «When a vaccine is safe». Nature. 439 (7076): 509. February 2006. Bibcode:2006Natur.439Q.509.. doi:10.1038/439509a. PMID 16452935.
- ↑ Arthritis and Lyme Disease Արխիվացված 4 Հոկտեմբեր 2013 Wayback Machine, WebMD Rheumatoid Arthritis Health Center, reviewed by David Zelman, MD on 1 October 2012.
- ↑ 21,0 21,1 disease 330178, բաժին Lyme disease(անգլ.) EMedicine կայքում
- ↑ Steere AC, Sikand VK, Schoen RT, Nowakowski J (August 2003). «Asymptomatic infection with Borrelia burgdorferi». Clinical Infectious Diseases. 37 (4): 528–32. doi:10.1086/376914. PMID 12905137. (primary source)
- ↑ 23,0 23,1 23,2 Biesiada G, Czepiel J, Leśniak MR, Garlicki A, Mach T (December 2012). «Lyme disease: review». Archives of Medical Science. 8 (6): 978–82. doi:10.5114/aoms.2012.30948. PMC 3542482. PMID 23319969.
- ↑ Aucott JN, Crowder LA, Yedlin V, Kortte KB (2012). «Bull's-Eye and Nontarget Skin Lesions of Lyme Disease: An Internet Survey of Identification of Erythema Migrans». Dermatology Research and Practice. 2012: 1–6. doi:10.1155/2012/451727. PMC 3485866. PMID 23133445.
{{cite journal}}: CS1 սպաս․ չպիտակված ազատ DOI (link) (primary source) - ↑ 25,0 25,1 25,2 25,3 Auwaerter PG, Aucott J, Dumler JS (January 2004). «Lyme borreliosis (Lyme disease): molecular and cellular pathobiology and prospects for prevention, diagnosis and treatment». Expert Reviews in Molecular Medicine. 6 (2): 1–22. doi:10.1017/S1462399404007276. PMID 14987414.
- ↑ Steere AC, Dhar A, Hernandez J, Fischer PA, Sikand VK, Schoen RT, Nowakowski J, McHugh G, Persing DH (January 2003). «Systemic symptoms without erythema migrans as the presenting picture of early Lyme disease». The American Journal of Medicine. 114 (1): 58–62. doi:10.1016/S0002-9343(02)01440-7. PMID 12543291. (primary source)
- ↑ Dandache P, Nadelman RB (June 2008). «Erythema migrans». Infectious Disease Clinics of North America. 22 (2): 235–60, vi. doi:10.1016/j.idc.2007.12.012. PMID 18452799.
- ↑ 28,0 28,1 Stanek G, Strle F (June 2008). «Lyme disease: European perspective». Infectious Disease Clinics of North America. 22 (2): 327–39, vii. doi:10.1016/j.idc.2008.01.001. PMID 18452805.
- ↑ Halperin JJ (June 2008). «Nervous system Lyme disease». Infectious Disease Clinics of North America. 22 (2): 261–74, vi. doi:10.1016/j.idc.2007.12.009. PMID 18452800.
- ↑ Chabria SB, Lawrason J (August 2007). «Altered mental status, an unusual manifestation of early disseminated Lyme disease: A case report». Journal of Medical Case Reports. 1: 62. doi:10.1186/1752-1947-1-62. PMC 1973078. PMID 17688693.
{{cite journal}}: CS1 սպաս․ չպիտակված ազատ DOI (link) - ↑ Stanek G, Wormser GP, Gray J, Strle F (February 2012). «Lyme borreliosis». Lancet. 379 (9814): 461–73. doi:10.1016/S0140-6736(11)60103-7. PMID 21903253.
- ↑ Nau R, Christen HJ, Eiffert H (January 2009). «Lyme disease--current state of knowledge». Deutsches Arzteblatt International. 106 (5): 72–81, quiz 82, I. doi:10.3238/arztebl.2009.0072. PMC 2695290. PMID 19562015.
- ↑ Bratton RL, Whiteside JW, Hovan MJ, Engle RL, Edwards FD (May 2008). «Diagnosis and treatment of Lyme disease». Mayo Clinic Proceedings. 83 (5): 566–71. doi:10.4065/83.5.566. PMID 18452688.
- ↑ Shadick NA, Phillips CB, Sangha O, Logigian EL, Kaplan RF, Wright EA, Fossel AH, Fossel K, Berardi V, Lew RA, Liang MH (December 1999). «Musculoskeletal and neurologic outcomes in patients with previously treated Lyme disease». Annals of Internal Medicine. 131 (12): 919–26. doi:10.7326/0003-4819-131-12-199912210-00003. PMID 10610642.
- ↑ Seltzer EG, Gerber MA, Cartter ML, Freudigman K, Shapiro ED (February 2000). «Long-term outcomes of persons with Lyme disease». JAMA. 283 (5): 609–16. doi:10.1001/jama.283.5.609. PMID 10665700.
- ↑ Fallon BA, Nields JA (November 1994). «Lyme disease: a neuropsychiatric illness». The American Journal of Psychiatry. 151 (11): 1571–83. doi:10.1176/ajp.151.11.1571. PMID 7943444.
- ↑ Hess A, Buchmann J, Zettl UK, Henschel S, Schlaefke D, Grau G, Benecke R (March 1999). «Borrelia burgdorferi central nervous system infection presenting as an organic schizophrenialike disorder». Biological Psychiatry. 45 (6): 795. doi:10.1016/S0006-3223(98)00277-7. PMID 10188012.
- ↑ Miklossy, J (2012). «Chronic or late lyme neuroborreliosis: analysis of evidence compared to chronic or late neurosyphilis». The Open Neurology Journal. 6: 146–57. doi:10.2174/1874205X01206010146. PMC 3551238. PMID 23346260.
- ↑ Puius YA, Kalish RA (June 2008). «Lyme arthritis: pathogenesis, clinical presentation, and management». Infectious Disease Clinics of North America. 22 (2): 289–300, vi–vii. doi:10.1016/j.idc.2007.12.014. PMID 18452802.
- ↑ Mullegger RR (2004). «Dermatological manifestations of Lyme borreliosis». European Journal of Dermatology. 14 (5): 296–309. PMID 15358567.
- ↑ Samuels DS, Radolf JD, eds. (2010). «Chapter 6, Structure, Function and Biogenesis of the Borrelia Cell Envelope». Borrelia: Molecular Biology, Host Interaction and Pathogenesis. Caister Academic Press. ISBN 978-1-904455-58-5.
- ↑ Cutler SJ, Ruzic-Sabljic E, Potkonjak A (February 2017). «Emerging borreliae - Expanding beyond Lyme borreliosis». Molecular and Cellular Probes. 31: 22–27. doi:10.1016/j.mcp.2016.08.003. PMID 27523487.
- ↑ Stanek G, Reiter M (April 2011). «The expanding Lyme Borrelia complex--clinical significance of genomic species?». Clinical Microbiology and Infection. 17 (4): 487–93. doi:10.1111/j.1469-0691.2011.03492.x. PMID 21414082.
- ↑ Schneider BS, Schriefer ME, Dietrich G, Dolan MC, Morshed MG, Zeidner NS (October 2008). «Borrelia bissettii isolates induce pathology in a murine model of disease». Vector Borne and Zoonotic Diseases. 8 (5): 623–33. doi:10.1089/vbz.2007.0251. PMID 18454594.
- ↑ Rudenko N, Golovchenko M, Mokrácek A, Piskunová N, Ruzek D, Mallatová N, Grubhoffer L (October 2008). «Detection of Borrelia bissettii in cardiac valve tissue of a patient with endocarditis and aortic valve stenosis in the Czech Republic». Journal of Clinical Microbiology. 46 (10): 3540–3. doi:10.1128/JCM.01032-08. PMC 2566110. PMID 18650352.
- ↑ 46,0 46,1 Tilly K, Rosa PA, Stewart PE (June 2008). «Biology of infection with Borrelia burgdorferi». Infectious Disease Clinics of North America. 22 (2): 217–34, v. doi:10.1016/j.idc.2007.12.013. PMC 2440571. PMID 18452798.
- ↑ 47,0 47,1 47,2 47,3 Ryan KJ, Ray CG, eds. (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. էջեր 434–37. ISBN 978-0-8385-8529-0.
- ↑ 2005 Fact Sheet, Prevent Tick Bites: Prevent Lyme Disease, Rutgers University, Rutgers Cooperative Research & Extension, New Jersey Agricultural Experiment Station, Deborah Smith-Fiola, Former Ocean County Agricultural Agent and George C. Hamilton, Ph.D., Extension Specialist in Pest Management, March 2005.
- ↑ 49,0 49,1 Lo Re V, Occi JL, MacGregor RR (April 2004). «Identifying the vector of Lyme disease». American Family Physician. 69 (8): 1935–7. PMID 15117014.
- ↑ «Westport Weston Health District». 2004. Արխիվացված է օրիգինալից 29 September 2013-ին. Վերցված է 26 September 2013-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Hovius JW, van Dam AP, Fikrig E (September 2007). «Tick-host-pathogen interactions in Lyme borreliosis». Trends in Parasitology. 23 (9): 434–8. doi:10.1016/j.pt.2007.07.001. PMID 17656156.
- ↑ 52,0 52,1 52,2 Steere AC, Coburn J, Glickstein L (April 2004). «The emergence of Lyme disease». The Journal of Clinical Investigation. 113 (8): 1093–101. doi:10.1172/JCI21681. PMC 385417. PMID 15085185.
- ↑ de Mik EL, van Pelt W, Docters-van Leeuwen BD, van der Veen A, Schellekens JF, Borgdorff MW (April 1997). «The geographical distribution of tick bites and erythema migrans in general practice in The Netherlands». International Journal of Epidemiology. 26 (2): 451–7. doi:10.1093/ije/26.2.451. PMID 9169184.
- ↑ Sun Y, Xu R (2003). «Ability of Ixodes persulcatus, Haemaphysalis concinna and Dermacentor silvarum ticks to acquire and transstadially transmit Borrelia garinii». Experimental & Applied Acarology. 31 (1–2): 151–60. doi:10.1023/B:APPA.0000005119.30172.43. PMID 14756409.
- ↑ Ledin KE, Zeidner NS, Ribeiro JM, Biggerstaff BJ, Dolan MC, Dietrich G, Vredevoe L, Piesman J (March 2005). «Borreliacidal activity of saliva of the tick Amblyomma americanum». Medical and Veterinary Entomology. 19 (1): 90–5. doi:10.1111/j.0269-283X.2005.00546.x. PMID 15752182.
- ↑ Masters EJ, Grigery CN, Masters RW (June 2008). «STARI, or Masters disease: Lone Star tick-vectored Lyme-like illness». Infectious Disease Clinics of North America. 22 (2): 361–76, viii. doi:10.1016/j.idc.2007.12.010. PMID 18452807.
- ↑ Clark K (November 2004). «Borrelia species in host-seeking ticks and small mammals in northern Florida». Journal of Clinical Microbiology. 42 (11): 5076–86. doi:10.1128/JCM.42.11.5076-5086.2004. PMC 525154. PMID 15528699.
- ↑ Eisen L, Eisen RJ, Lane RS (December 2004). «The roles of birds, lizards, and rodents as hosts for the western black-legged tick Ixodes pacificus». Journal of Vector Ecology. 29 (2): 295–308. PMID 15709249.
- ↑ 59,0 59,1 Lane RS, Mun J, Eisen L, Eisen RJ (August 2006). «Refractoriness of the western fence lizard (Sceloporus occidentalis) to the Lyme disease group spirochete Borrelia bissettii». The Journal of Parasitology. 92 (4): 691–6. doi:10.1645/GE-738R1.1. PMID 16995383.
- ↑ Walsh CA, Mayer EW, Baxi LV (January 2007). «Lyme disease in pregnancy: case report and review of the literature». Obstetrical & Gynecological Survey. 62 (1): 41–50. doi:10.1097/01.ogx.0000251024.43400.9a. PMID 17176487.
- ↑ Dotters-Katz, S; Kuller, J; Heine, P (September 2013). «Arthropod-Borne Bacterial Diseases in Pregnancy». Obstetrical & Gynecological Survey. 68 (9): 41–50. doi:10.1097/OGX.0b013e3182a5ed46. PMID 25102120.
- ↑ Lakos A, Solymosi N (June 2010). «Maternal Lyme borreliosis and pregnancy outcome». International Journal of Infectious Diseases. 14 (6): e494–8. doi:10.1016/j.ijid.2009.07.019. PMID 19926325.
- ↑ Steere A (August 31, 1989). «Medical Progress, Lyme Disease». The New England Journal of Medicine. 321 (9): 586–596. doi:10.1056/NEJM198908313210906. PMID 2668764.
- ↑ «Tick Attachment and Tickborne Diseases». www.maine.gov.
- ↑ Magnarelli LA, Anderson JF (August 1988). «Ticks and biting insects infected with the etiologic agent of Lyme disease, Borrelia burgdorferi». Journal of Clinical Microbiology. 26 (8): 1482–6. PMC 266646. PMID 3170711.
- ↑ Luger SW (June 1990). «Lyme disease transmitted by a biting fly». The New England Journal of Medicine. 322 (24): 1752. doi:10.1056/NEJM199006143222415. PMID 2342543.
- ↑ Bach G (2001). «Recovery of Lyme spirochetes by PCR in semen samples of previously diagnosed Lyme disease patients». 14th International Scientific Conference on Lyme Disease. Արխիվացված է օրիգինալից 20 June 2006-ին.
{{cite conference}}: Unknown parameter|booktitle=ignored (|book-title=suggested) (օգնություն); Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Schmidt BL, Aberer E, Stockenhuber C, Klade H, Breier F, Luger A (March 1995). «Detection of Borrelia burgdorferi DNA by polymerase chain reaction in the urine and breast milk of patients with Lyme borreliosis». Diagnostic Microbiology and Infectious Disease. 21 (3): 121–8. doi:10.1016/0732-8893(95)00027-8. PMID 7648832.
- ↑ «CDC Lyme FAQ». Centers for Disease Control. 2018-07-19. Արխիվացված է օրիգինալից 26 March 2013-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Swanson SJ, Neitzel D, Reed KD, Belongia EA (October 2006). «Coinfections acquired from ixodes ticks». Clinical Microbiology Reviews. 19 (4): 708–27. doi:10.1128/CMR.00011-06. PMC 1592693. PMID 17041141.
- ↑ Wormser GP (June 2006). «Clinical practice. Early Lyme disease». The New England Journal of Medicine. 354 (26): 2794–801. doi:10.1056/NEJMcp061181. PMID 16807416.
- ↑ Lindgren E, Gustafson R (July 2001). «Tick-borne encephalitis in Sweden and climate change». Lancet. 358 (9275): 16–8. doi:10.1016/S0140-6736(00)05250-8. PMID 11454371.
- ↑ Varde S, Beckley J, Schwartz I (1998). «Prevalence of tick-borne pathogens in Ixodes scapularis in a rural New Jersey County». Emerging Infectious Diseases. 4 (1): 97–9. doi:10.3201/eid0401.980113. PMC 2627663. PMID 9452402.
- ↑ Pachner AR, Steiner I (June 2007). «Lyme neuroborreliosis: infection, immunity, and inflammation». The Lancet. Neurology. 6 (6): 544–52. doi:10.1016/S1474-4422(07)70128-X. PMID 17509489.
- ↑ Fikrig E, Narasimhan S (April 2006). «Borrelia burgdorferi--traveling incognito?». Microbes and Infection. 8 (5): 1390–9. doi:10.1016/j.micinf.2005.12.022. PMID 16698304.
- ↑ Xu Q, Seemanapalli SV, Reif KE, Brown CR, Liang FT (April 2007). «Increasing the recruitment of neutrophils to the site of infection dramatically attenuates Borrelia burgdorferi infectivity». Journal of Immunology. 178 (8): 5109–15. doi:10.4049/jimmunol.178.8.5109. PMID 17404293.
- ↑ Coleman JL, Gebbia JA, Piesman J, Degen JL, Bugge TH, Benach JL (June 1997). «Plasminogen is required for efficient dissemination of B. burgdorferi in ticks and for enhancement of spirochetemia in mice». Cell. 89 (7): 1111–9. doi:10.1016/S0092-8674(00)80298-6. PMID 9215633.
- ↑ Steere AC (July 2001). «Lyme disease». The New England Journal of Medicine. 345 (2): 115–25. doi:10.1056/NEJM200107123450207. PMID 11450660.
- ↑ Rupprecht TA, Koedel U, Fingerle V, Pfister HW (2008). «The pathogenesis of lyme neuroborreliosis: from infection to inflammation». Molecular Medicine. 14 (3–4): 205–12. doi:10.2119/2007-00091.Rupprecht (inactive 2018-10-28). PMC 2148032. PMID 18097481. Արխիվացված է օրիգինալից 3 April 2015-ին.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն)CS1 սպաս․ DOI inactive as of Հոկտեմբեր 2018 (link) - ↑ Cabello FC, Godfrey HP, Newman SA (August 2007). «Hidden in plain sight: Borrelia burgdorferi and the extracellular matrix». Trends in Microbiology. 15 (8): 350–4. doi:10.1016/j.tim.2007.06.003. PMID 17600717.
- ↑ Ramesh G, Alvarez AL, Roberts ED, Dennis VA, Lasater BL, Alvarez X, Philipp MT (September 2003). «Pathogenesis of Lyme neuroborreliosis: Borrelia burgdorferi lipoproteins induce both proliferation and apoptosis in rhesus monkey astrocytes». European Journal of Immunology. 33 (9): 2539–50. doi:10.1002/eji.200323872. PMID 12938230.
- ↑ Halperin JJ, Heyes MP (January 1992). «Neuroactive kynurenines in Lyme borreliosis». Neurology. 42 (1): 43–50. doi:10.1212/WNL.42.1.43. PMID 1531156.
- ↑ Fallon BA, Keilp J, Prohovnik I, Heertum RV, Mann JJ (2003). «Regional cerebral blood flow and cognitive deficits in chronic lyme disease». The Journal of Neuropsychiatry and Clinical Neurosciences. 15 (3): 326–32. doi:10.1176/appi.neuropsych.15.3.326. PMID 12928508.
- ↑ Gasse T, Murr C, Meyersbach P, Schmutzhard E, Wachter H, Fuchs D (September 1994). «Neopterin production and tryptophan degradation in acute Lyme neuroborreliosis versus late Lyme encephalopathy». European Journal of Clinical Chemistry and Clinical Biochemistry (Submitted manuscript). 32 (9): 685–9. doi:10.1515/cclm.1994.32.9.685. PMID 7865624.
- ↑ Zajkowska J, Grygorczuk S, Kondrusik M, Pancewicz S, Hermanowska-Szpakowicz T (2006). «[New aspects of pathogenesis of Lyme borreliosis]». Przeglad Epidemiologiczny (Polish). 60 Suppl 1 (Suppl 1): 167–70. PMID 16909797.
{{cite journal}}: CS1 սպաս․ չճանաչված լեզու (link) - ↑ Ercolini AM, Miller SD (January 2009). «The role of infections in autoimmune disease». Clinical and Experimental Immunology. 155 (1): 1–15. doi:10.1111/j.1365-2249.2008.03834.x. PMC 2665673. PMID 19076824.
- ↑ Singh SK, Girschick HJ (July 2004). «Lyme borreliosis: from infection to autoimmunity». Clinical Microbiology and Infection. 10 (7): 598–614. doi:10.1111/j.1469-0691.2004.00895.x. PMID 15214872.
- ↑ Oldstone MB (October 1998). «Molecular mimicry and immune-mediated diseases» (PDF). FASEB Journal. 12 (13): 1255–65. PMID 9761770.
- ↑ Raveche ES, Schutzer SE, Fernandes H, Bateman H, McCarthy BA, Nickell SP, Cunningham MW (February 2005). «Evidence of Borrelia autoimmunity-induced component of Lyme carditis and arthritis». Journal of Clinical Microbiology. 43 (2): 850–6. doi:10.1128/JCM.43.2.850-856.2005. PMC 548028. PMID 15695691.
- ↑ Weinstein A, Britchkov M (July 2002). «Lyme arthritis and post-Lyme disease syndrome». Current Opinion in Rheumatology. 14 (4): 383–7. doi:10.1097/00002281-200207000-00008. PMID 12118171.
- ↑ Bolz DD, Weis JJ (August 2004). «Molecular mimicry to Borrelia burgdorferi: pathway to autoimmunity?». Autoimmunity. 37 (5): 387–92. doi:10.1080/08916930410001713098. PMID 15621562.
- ↑ Wormser GP, Masters E, Nowakowski J, McKenna D, Holmgren D, Ma K, Ihde L, Cavaliere LF, Nadelman RB (October 2005). «Prospective clinical evaluation of patients from Missouri and New York with erythema migrans-like skin lesions». Clinical Infectious Diseases. 41 (7): 958–65. doi:10.1086/432935. PMID 16142659.
- ↑ Brown SL, Hansen SL, Langone JJ (July 1999). «Role of serology in the diagnosis of Lyme disease». JAMA. 282 (1): 62–6. doi:10.1001/jama.282.1.62. PMID 10404913.
- ↑ Hofmann H (1996). «Lyme borreliosis--problems of serological diagnosis». Infection. 24 (6): 470–2. doi:10.1007/BF01713052. PMID 9007597.
- ↑ Pachner AR (1989). «Neurologic manifestations of Lyme disease, the new "great imitator"». Reviews of Infectious Diseases. 11 Suppl 6: S1482–6. doi:10.1093/clinids/11.Supplement_6.S1482. PMID 2682960.
- ↑ Branda JA, Linskey K, Kim YA, Steere AC, Ferraro MJ (September 2011). «Two-tiered antibody testing for Lyme disease with use of 2 enzyme immunoassays, a whole-cell sonicate enzyme immunoassay followed by a VlsE C6 peptide enzyme immunoassay». Clinical Infectious Diseases. 53 (6): 541–7. doi:10.1093/cid/cir464. PMID 21865190.
- ↑ «Lyme disease diagnosis». Centers for Disease Control and Prevention (CDC). 7 October 2008. Արխիվացված է օրիգինալից 28 August 2009-ին. Վերցված է 6 July 2009-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ 98,0 98,1 Wormser GP, Dattwyler RJ, Shapiro ED, Halperin JJ, Steere AC, Klempner MS, Krause PJ, Bakken JS, Strle F, Stanek G, Bockenstedt L, Fish D, Dumler JS, Nadelman RB (November 2006). «The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America» (PDF). Clinical Infectious Diseases. 43 (9): 1089–134. doi:10.1086/508667. PMID 17029130. Արխիվացված է օրիգինալից (PDF) 27 November 2014-ին.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Wilske B (2005). «Epidemiology and diagnosis of Lyme borreliosis». Annals of Medicine. 37 (8): 568–79. doi:10.1080/07853890500431934. PMID 16338759.
- ↑ Engstrom SM, Shoop E, Johnson RC (February 1995). «Immunoblot interpretation criteria for serodiagnosis of early Lyme disease». Journal of Clinical Microbiology. 33 (2): 419–27. PMC 227960. PMID 7714202.
- ↑ Sivak SL, Aguero-Rosenfeld ME, Nowakowski J, Nadelman RB, Wormser GP (October 1996). «Accuracy of IgM immunoblotting to confirm the clinical diagnosis of early Lyme disease». Archives of Internal Medicine. 156 (18): 2105–9. doi:10.1001/archinte.156.18.2105. PMID 8862103.
- ↑ 102,0 102,1 Steere AC, McHugh G, Damle N, Sikand VK (July 2008). «Prospective study of serologic tests for lyme disease». Clinical Infectious Diseases. 47 (2): 188–95. doi:10.1086/589242. PMC 5538270. PMID 18532885.
- ↑ Goossens HA, Nohlmans MK, van den Bogaard AE (1999). «Epstein-Barr virus and cytomegalovirus infections cause false-positive results in IgM two-test protocol for early Lyme borreliosis». Infection. 27 (3): 231. doi:10.1007/BF02561539. PMID 10378140.
- ↑ Strasfeld L, Romanzi L, Seder RH, Berardi VP (December 2005). «False-positive serological test results for Lyme disease in a patient with acute herpes simplex virus type 2 infection». Clinical Infectious Diseases. 41 (12): 1826–7. doi:10.1086/498319. PMID 16288417.
- ↑ Molloy PJ, Persing DH, Berardi VP (August 2001). «False-positive results of PCR testing for Lyme disease». Clinical Infectious Diseases. 33 (3): 412–3. doi:10.1086/321911. PMID 11438915.
- ↑ 106,0 106,1 Aguero-Rosenfeld ME, Wang G, Schwartz I, Wormser GP (July 2005). «Diagnosis of lyme borreliosis». Clinical Microbiology Reviews. 18 (3): 484–509. doi:10.1128/CMR.18.3.484-509.2005. PMC 1195970. PMID 16020686.
- ↑ Nocton JJ, Dressler F, Rutledge BJ, Rys PN, Persing DH, Steere AC (January 1994). «Detection of Borrelia burgdorferi DNA by polymerase chain reaction in synovial fluid from patients with Lyme arthritis». The New England Journal of Medicine. 330 (4): 229–34. doi:10.1056/NEJM199401273300401. PMID 8272083.
- ↑ Hyde FW, Johnson RC, White TJ, Shelburne CE (January 1989). «Detection of antigens in urine of mice and humans infected with Borrelia burgdorferi, etiologic agent of Lyme disease». Journal of Clinical Microbiology. 27 (1): 58–61. PMC 267232. PMID 2913036.
- ↑ Shafagati N, Patanarut A, Luchini A, Lundberg L, Bailey C, Petricoin E, Liotta L, Narayanan A, Lepene B, Kehn-Hall K (July 2014). «The use of Nanotrap particles for biodefense and emerging infectious disease diagnostics». Pathogens and Disease. 71 (2): 164–76. doi:10.1111/2049-632X.12136. PMID 24449537.
- ↑ Shafagati N, Patanarut A, Luchini A, Lundberg L, Bailey C, Petricoin E, Liotta L, Narayanan A, Lepene B, Kehn-Hall K (July 2014). «The use of Nanotrap particles for biodefense and emerging infectious disease diagnostics». Pathogens and Disease. 71 (2): 164–76. doi:10.1111/2049-632x.12136. PMID 24449537.
- ↑ Burdash N, Fernandes J (June 1991). «Lyme borreliosis: detecting the great imitator». The Journal of the American Osteopathic Association. 91 (6): 573–4, 577–8. PMID 1874654.
- ↑ Coyle PK, Schutzer SE, Deng Z, Krupp LB, Belman AL, Benach JL, Luft BJ (November 1995). «Detection of Borrelia burgdorferi-specific antigen in antibody-negative cerebrospinal fluid in neurologic Lyme disease». Neurology. 45 (11): 2010–5. doi:10.1212/WNL.45.11.2010. PMID 7501150.
- ↑ Valentine-Thon E, Ilsemann K, Sandkamp M (January 2007). «A novel lymphocyte transformation test (LTT-MELISA) for Lyme borreliosis». Diagnostic Microbiology and Infectious Disease. 57 (1): 27–34. doi:10.1016/j.diagmicrobio.2006.06.008. PMID 16876371.
- ↑ von Baehr V, Doebis C, Volk HD, von Baehr R (October 2012). «The lymphocyte transformation test for borrelia detects active lyme borreliosis and verifies effective antibiotic treatment». The Open Neurology Journal. 6 (2): 104–12. doi:10.2174/1874205X01206010104. PMC 3474945. PMID 23091571.
- ↑ Puri BK, Segal DR, Monro JA (December 2014). «Diagnostic use of the lymphocyte transformation test-memory lymphocyte immunostimulation assay in confirming active Lyme borreliosis in clinically and serologically ambiguous cases». International Journal of Clinical and Experimental Medicine. 7 (12): 5890–2. PMC 4307574. PMID 25664127.
- ↑ Eisendle K, Grabner T, Zelger B (February 2007). «Focus floating microscopy: "gold standard" for cutaneous borreliosis?». American Journal of Clinical Pathology. 127 (2): 213–22. doi:10.1309/3369XXFPEQUNEP5C. PMID 17210530.
- ↑ Cadavid D (November 2006). «The mammalian host response to borrelia infection». Wiener Klinische Wochenschrift. 118 (21–22): 653–8. doi:10.1007/s00508-006-0692-0. PMID 17160603.
- ↑ Hildenbrand P, Craven DE, Jones R, Nemeskal P (June 2009). «Lyme neuroborreliosis: manifestations of a rapidly emerging zoonosis». AJNR. American Journal of Neuroradiology. 30 (6): 1079–87. doi:10.3174/ajnr.A1579. PMID 19346313.
- ↑ Westervelt HJ, McCaffrey RJ (September 2002). «Neuropsychological functioning in chronic Lyme disease». Neuropsychology Review. 12 (3): 153–77. doi:10.1023/A:1020381913563. PMID 12428915.
- ↑ «CDC - Lyme Disease - NIOSH Workplace Safety and Health Topic». www.cdc.gov. 2017-08-03. Արխիվացված է օրիգինալից 13 November 2015-ին. Վերցված է 3 November 2015-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Centers for Disease Control and Prevention. «Avoid bug bites». Արխիվացված է օրիգինալից 13 March 2016-ին. Վերցված է 15 March 2016-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Rand PW, Lubelczyk C, Holman MS, Lacombe EH, Smith RP (July 2004). «Abundance of Ixodes scapularis (Acari: Ixodidae) after the complete removal of deer from an isolated offshore island, endemic for Lyme Disease». Journal of Medical Entomology. 41 (4): 779–84. doi:10.1603/0022-2585-41.4.779. PMID 15311475.
- ↑ «Figure 2: Changes in deer density and cases of Lyme disease in Mumford Cove, Connecticut, 1996–2004 (CT DEP data)». Managing Urban Deer in Connecticut (PDF) (2nd ed.). Connecticut Department of Environmental Protection - Wildlife Division. June 2007. էջ 4. Արխիվացված է օրիգինալից (PDF) 2 June 2013-ին.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Perkins SE, Cattadori IM, Tagliapietra V, Rizzoli AP, Hudson PJ (August 2006). «Localized deer absence leads to tick amplification». Ecology. 87 (8): 1981–6. CiteSeerX 10.1.1.218.7660. doi:10.1890/0012-9658(2006)87[1981:LDALTT]2.0.CO;2. PMID 16937637.
- ↑ Stafford, Kirby C. (2004). Tick Management Handbook (PDF). Connecticut Agricultural Experiment Station and Connecticut Department of Public Health. էջ 46. Արխիվացված է օրիգինալից (PDF) 25 October 2007-ին. Վերցված է 21 August 2007-ին.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Staub D, Debrunner M, Amsler L, Steffen R (2002). «Effectiveness of a repellent containing DEET and EBAAP for preventing tick bites». Wilderness & Environmental Medicine. 13 (1): 12–20. doi:10.1580/1080-6032(2002)013[0012:EOARCD]2.0.CO;2. PMID 11929056.
- ↑ 127,0 127,1 Gern L, Estrada-Peña A, Frandsen F, Gray JS, Jaenson TG, Jongejan F, Kahl O, Korenberg E, Mehl R, Nuttall PA (March 1998). «European reservoir hosts of Borrelia burgdorferi sensu lato». Zentralblatt Fur Bakteriologie. 287 (3): 196–204. doi:10.1016/S0934-8840(98)80121-7. PMID 9580423.
- ↑ 128,0 128,1 Wodecka, Beata; Rymaszewska, Anna; Skotarczak, Bogumila (2013). «Host and pathogen DNA identification in blood meals of nymphal Ixodes ricinus ticks from forest parks and rural forests of Poland». Experimental and Applied Acarology. 62 (4): 543–555. doi:10.1007/s10493-013-9763-x. PMC 3933768. PMID 24352572.
- ↑ Jaenson TG, Tälleklint L (September 1992). «Incompetence of roe deer as reservoirs of the Lyme borreliosis spirochete». Journal of Medical Entomology. 29 (5): 813–7. doi:10.1093/jmedent/29.5.813. PMID 1404260.
- ↑ Tälleklint L, Jaenson TG (1994). «Transmission of Borrelia burgdorferi sl from mammal reservoirs to the primary vector of Lyme borreliosis, Ixodes ricinus (Acari: Ixodidae), in Sweden». J. Med. Entomol. 31 (6): 880–886. doi:10.1093/jmedent/31.6.880.
- ↑ 131,0 131,1 Wodecka B, Rymaszewska A, Skotarczak B (April 2014). «Host and pathogen DNA identification in blood meals of nymphal Ixodes ricinus ticks from forest parks and rural forests of Poland». Experimental & Applied Acarology. 62 (4): 543–55. doi:10.1007/s10493-013-9763-x. PMC 3933768. PMID 24352572.
- ↑ Overzier E, Pfister K, Herb I, Mahling M, Böck G, Silaghi C (June 2013). «Detection of tick-borne pathogens in roe deer (Capreolus capreolus), in questing ticks (Ixodes ricinus), and in ticks infesting roe deer in southern Germany». Ticks and Tick-Borne Diseases. 4 (4): 320–8. doi:10.1016/j.ttbdis.2013.01.004. PMID 23571115.
- ↑ Poland GA, Jacobson RM (March 2001). «The prevention of Lyme disease with vaccine». Vaccine. 19 (17–19): 2303–8. doi:10.1016/S0264-410X(00)00520-X. PMID 11257352.
- ↑ Rowe, Claudia (13 June 1999). «Lukewarm Response To New Lyme Vaccine». The New York Times. Արխիվացված է օրիգինալից 10 February 2012-ին. Վերցված է 11 July 2008-ին.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ 135,0 135,1 135,2 Abbott A (February 2006). «Lyme disease: uphill struggle». Nature. 439 (7076): 524–5. doi:10.1038/439524a. PMID 16452949.
- ↑ «Sole Lyme Vaccine Is Pulled Off Market». The New York Times. 28 February 2002. Արխիվացված է օրիգինալից 30 August 2010-ին. Վերցված է 11 July 2008-ին.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ 137,0 137,1 Nigrovic LE, Thompson KM (January 2007). «The Lyme vaccine: a cautionary tale». Epidemiology and Infection. 135 (1): 1–8. doi:10.1017/S0950268806007096. PMC 2870557. PMID 16893489.
- ↑ 138,0 138,1 Brooks, DVM, Wendy C. «Lyme Disease». Veterinary Information Network. Վերցված է 10 February 2012-ին.
- ↑ «Anti-vaxxers stopped the last Lyme disease vaccine. The FDA has just fast-tracked a new one». Newsweek. 25 July 2017. Վերցված է 25 December 2017-ին.
- ↑ 140,0 140,1 Piesman J, Dolan MC (May 2002). «Protection against lyme disease spirochete transmission provided by prompt removal of nymphal Ixodes scapularis (Acari: Ixodidae)». Journal of Medical Entomology. 39 (3): 509–12. doi:10.1603/0022-2585-39.3.509. PMID 12061448.
- ↑ «Tickbitepreventionweek». Արխիվացված է օրիգինալից 5 June 2014-ին. Վերցված է 2014-06-05-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Zeller JL, Burke AE, Glass RM (June 2007). «JAMA patient page. Lyme disease». JAMA. 297 (23): 2664. doi:10.1001/jama.297.23.2664. PMID 17579234.
- ↑ «Tick Allergy». 2014. Արխիվացված է օրիգինալից 14 May 2015-ին. Վերցված է 30 April 2015-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ 144,00 144,01 144,02 144,03 144,04 144,05 144,06 144,07 144,08 144,09 144,10 144,11 144,12 144,13 144,14 144,15 Wright WF, Riedel DJ, Talwani R, Gilliam BL (June 2012). «Diagnosis and management of Lyme disease». American Family Physician. 85 (11): 1086–93. PMID 22962880. Արխիվացված է օրիգինալից 27 September 2013-ին.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ «Lyme disease». The Centers for Disease Control and Prevention. 12 October 2016. Արխիվացված է օրիգինալից 17 June 2017-ին. Վերցված է 22 June 2017-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) Այս հոդվածը պարունակում է , աղբյուր՝ կայք կամ փաստաթուղթ՝ Centers for Disease Control and Prevention.
Այս հոդվածը պարունակում է , աղբյուր՝ կայք կամ փաստաթուղթ՝ Centers for Disease Control and Prevention.
- ↑ Berende A, ter Hofstede HJ, Vos FJ, van Middendorp H, Vogelaar ML, Tromp M, van den Hoogen FH, Donders AR, Evers AW, Kullberg BJ (March 2016). «Randomized Trial of Longer-Term Therapy for Symptoms Attributed to Lyme Disease». The New England Journal of Medicine. 374 (13): 1209–20. doi:10.1056/NEJMoa1505425. PMID 27028911.
- ↑ Krause PJ, Foley DT, Burke GS, Christianson D, Closter L, Spielman A (December 2006). «Reinfection and relapse in early Lyme disease». The American Journal of Tropical Medicine and Hygiene. 75 (6): 1090–4. PMID 17172372.
- ↑ Bope, Edward T.; Kellerman, Rick D. (2012). Conn's Current Therapy 2013: Expert Consult: Online. Elsevier Health Sciences. էջ 151. ISBN 978-1455733347. Արխիվացված է օրիգինալից 8 September 2017-ին.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (օգնություն) - ↑ «Post-Treatment Lyme Disease Syndrome» (English). CDC. 3 November 2016. Արխիվացված է օրիգինալից 17 June 2017-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն)CS1 սպաս․ չճանաչված լեզու (link) - ↑ «Glomerular Disease». The Merck Veterinary Manual. Արխիվացված է օրիգինալից 26 June 2017-ին. Վերցված է 19 May 2017-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Staubinger, PhD, R. (2000-05-31). «Lyme Disease». Sirius Dog. Արխիվացված է օրիգինալից 23 June 2012-ին. Վերցված է 10 February 2012-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն)Կաղապար:Unreliable source? - ↑ Fatal cases of Lyme disease reported in the medical literature include:
- Kirsch M, Ruben FL, Steere AC, Duray PH, Norden CW, Winkelstein A (May 1988). «Fatal adult respiratory distress syndrome in a patient with Lyme disease». JAMA. 259 (18): 2737–9. doi:10.1001/jama.1988.03720180063034. PMID 3357244.
- Oksi J, Kalimo H, Marttila RJ, Marjamäki M, Sonninen P, Nikoskelainen J, Viljanen MK (December 1996). «Inflammatory brain changes in Lyme borreliosis. A report on three patients and review of literature». Brain. 119 ( Pt 6) (Pt 6): 2143–54. doi:10.1093/brain/119.6.2143. PMID 9010017.
- Waniek C, Prohovnik I, Kaufman MA, Dwork AJ (1995). «Rapidly progressive frontal-type dementia associated with Lyme disease». The Journal of Neuropsychiatry and Clinical Neurosciences. 7 (3): 345–7. doi:10.1176/jnp.7.3.345. PMID 7580195.
- Cary NR, Fox B, Wright DJ, Cutler SJ, Shapiro LM, Grace AA (February 1990). «Fatal Lyme carditis and endodermal heterotopia of the atrioventricular node». Postgraduate Medical Journal. 66 (772): 134–6. doi:10.1136/pgmj.66.772.134. PMC 2429516. PMID 2349186.
- ↑ Higgins R (August 2004). «Emerging or re-emerging bacterial zoonotic diseases: bartonellosis, leptospirosis, Lyme borreliosis, plague». Revue Scientifique et Technique. 23 (2): 569–81. doi:10.20506/rst.23.2.1503. PMID 15702720.
- ↑ Bouattour A, Ghorbel A, Chabchoub A, Postic D (2004). «[Lyme borreliosis situation in North Africa]» [Lyme borreliosis situation in North Africa]. Archives de l'Institut Pasteur de Tunis (French). 81 (1–4): 13–20. PMID 16929760.
{{cite journal}}: CS1 սպաս․ չճանաչված լեզու (link) - ↑ Dsouli N, Younsi-Kabachii H, Postic D, Nouira S, Gern L, Bouattour A (July 2006). «Reservoir role of lizard Psammodromus algirus in transmission cycle of Borrelia burgdorferi sensu lato (Spirochaetaceae) in Tunisia». Journal of Medical Entomology. 43 (4): 737–42. doi:10.1603/0022-2585(2006)43[737:RROLPA]2.0.CO;2. PMID 16892633.
- ↑ Helmy N (August 2000). «Seasonal abundance of Ornithodoros (O.) savignyi and prevalence of infection with Borrelia spirochetes in Egypt». Journal of the Egyptian Society of Parasitology. 30 (2): 607–19. PMID 10946521.
- ↑ Fivaz BH, Petney TN (September 1989). «Lyme disease--a new disease in southern Africa?». Journal of the South African Veterinary Association. 60 (3): 155–8. PMID 2699499.
- ↑ Jowi JO, Gathua SN (May 2005). «Lyme disease: report of two cases». East African Medical Journal. 82 (5): 267–9. doi:10.4314/eamj.v82i5.9318. PMID 16119758.
- ↑ Li M, Masuzawa T, Takada N, Ishiguro F, Fujita H, Iwaki A, Wang H, Wang J, Kawabata M, Yanagihara Y (July 1998). «Lyme disease Borrelia species in northeastern China resemble those isolated from far eastern Russia and Japan». Applied and Environmental Microbiology. 64 (7): 2705–9. PMC 106449. PMID 9647853.
- ↑ Masuzawa T (December 2004). «Terrestrial distribution of the Lyme borreliosis agent Borrelia burgdorferi sensu lato in East Asia». Japanese Journal of Infectious Diseases. 57 (6): 229–35. PMID 15623946. Արխիվացված է օրիգինալից 22 January 2013-ին.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Walder G, Lkhamsuren E, Shagdar A, Bataa J, Batmunkh T, Orth D, Heinz FX, Danichova GA, Khasnatinov MA, Würzner R, Dierich MP (May 2006). «Serological evidence for tick-borne encephalitis, borreliosis, and human granulocytic anaplasmosis in Mongolia». International Journal of Medical Microbiology. 296 Suppl 40: 69–75. doi:10.1016/j.ijmm.2006.01.031. PMID 16524782.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (օգնություն) - ↑ Rizzoli A, Hauffe H, Carpi G, Vourc HG, Neteler M, Rosa R (July 2011). «Lyme borreliosis in Europe». Euro Surveillance. 16 (27). PMID 21794218. Արխիվացված է օրիգինալից 9 July 2011-ին.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Smith R, Takkinen J (June 2006). «Lyme borreliosis: Europe-wide coordinated surveillance and action needed?». Euro Surveillance. 11 (6): E060622.1. PMID 16819127. Արխիվացված է օրիգինալից 17 June 2012-ին.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Lopes de Carvalho I, Núncio MS (2006). «Laboratory diagnosis of Lyme borreliosis at the Portuguese National Institute of Health (1990-2004)». Euro Surveillance. 11 (10): 257–60. PMID 17130658. Արխիվացված է օրիգինալից 17 June 2012-ին.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ 165,0 165,1 165,2 165,3 «Epidemiology of Lyme borreliosis in the UK». HPA. Արխիվացված է օրիգինալից 10 June 2013-ին. Վերցված է 15 December 2012-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Muhlemann MF, Wright DJ (January 1987). «Emerging pattern of Lyme disease in the United Kingdom and Irish Republic». Lancet. 1 (8527): 260–2. doi:10.1016/S0140-6736(87)90074-2. PMID 2880076.
- ↑ 167,0 167,1 Lyme Disease Արխիվացված 15 Հունիս 2013 Wayback Machine Hansard 11 November 1991
- ↑ 168,0 168,1 «Tick Lyme disease off your holiday list» (Press release). Health Protection Agency. 14 April 2011. Արխիվացված է օրիգինալից 28 April 2011-ին. Վերցված է 29 March 2013-ին.
{{cite press release}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ «Concern about rise in Lyme disease cases». Lyme Disease Action. 15 December 2011. Արխիվացված է օրիգինալից 19 June 2013-ին. Վերցված է 15 December 2012-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Cassidy, Frank (14 March 2011). «Tayside revealed as a Lyme disease hotspot as cases soar». Press and Journal. Արխիվացված է օրիգինալից 11 March 2016-ին.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ «Lyme disease: A clear and present danger». RCN. 28 April 2009. Արխիվացված է օրիգինալից 29 March 2013-ին. Վերցված է 15 December 2012-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ «Guidance on Part 2 - Notifiable Diseases, Notifiable Organisms and Health Risk States». Scotland.gov.uk. 10 September 2012. Վերցված է 15 December 2012-ին.
- ↑ Lyme Disease Արխիվացված 15 Հունիս 2013 Wayback Machine Hansard, 3 February 1997
- ↑ Tick-Borne Disease, Risk and Realit Արխիվացված 20 Նոյեմբեր 2012 Wayback Machine BADA-UK, Wendy Fox, 2010
- ↑ «Lyme borreliosis epidemiology and surveillance: May 2013». HPA. Արխիվացված է օրիգինալից 25 November 2015-ին. Վերցված է 24 November 2015-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ «Zoonoses report UK 2009» (PDF). DEFRA. 24 January 2011. Արխիվացված է օրիգինալից (PDF) 3 November 2012-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Overview Tick Bite Prevention Week Արխիվացված 10 Ապրիլ 2012 Wayback Machine
- ↑ Haywood GA, O'Connell S, Gray HH (July 1993). «Lyme carditis: a United Kingdom perspective». British Heart Journal. 70 (1): 15–6. doi:10.1136/hrt.70.1.15. PMC 1025222. PMID 8037992.
- ↑ Guy EC, Bateman DE, Martyn CN, Heckels JE, Lawton NF (March 1989). «Lyme disease: prevalence and clinical importance of Borrelia burgdorferi specific IgG in forestry workers». Lancet. 1 (8636): 484–6. doi:10.1016/S0140-6736(89)91377-9. PMID 2563850.
- ↑ Smith FD, Ballantyne R, Morgan ER, Wall R (March 2012). «Estimating Lyme disease risk using pet dogs as sentinels». Comparative Immunology, Microbiology and Infectious Diseases. 35 (2): 163–7. doi:10.1016/j.cimid.2011.12.009. PMID 22257866.
{{cite journal}}: Unknown parameter|laydate=ignored (օգնություն); Unknown parameter|laysource=ignored (օգնություն); Unknown parameter|laysummary=ignored (օգնություն) - ↑ Roberts, Michelle (24 January 2012). «Lyme disease risk from dogs 'higher than thought'». BBC News. Արխիվացված է օրիգինալից 31 January 2012-ին.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ «The London climate change adaptation strategy - Draft report» (PDF). Greater London Authority. August 2008. Արխիվացված է օրիգինալից (PDF) 17 August 2012-ին.
- ↑ Brownstein JS, Holford TR, Fish D (March 2005). «Effect of Climate Change on Lyme Disease Risk in North America». EcoHealth. 2 (1): 38–46. doi:10.1007/s10393-004-0139-x. PMC 2582486. PMID 19008966.
- ↑ 184,0 184,1 Killilea ME, Swei A, Lane RS, Briggs CJ, Ostfeld RS (June 2008). «Spatial dynamics of lyme disease: a review» (PDF). EcoHealth. 5 (2): 167–95. CiteSeerX 10.1.1.580.8928. doi:10.1007/s10393-008-0171-3. PMID 18787920. Արխիվացված է օրիգինալից (PDF) 8 September 2015-ին.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ BC Ministry of Agriculture. «Ticks and Humans in British Columbia». Agf.gov.bc.ca. Արխիվացված է օրիգինալից 3 January 2013-ին. Վերցված է 15 December 2012-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ «Lyme Disease Fact Sheet». Phac-aspc.gc.ca. 4 July 2012. Արխիվացված է օրիգինալից 27 December 2012-ին. Վերցված է 15 December 2012-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Ogden NH, Lindsay LR, Morshed M, Sockett PN, Artsob H (June 2009). «The emergence of Lyme disease in Canada». CMAJ. 180 (12): 1221–4. doi:10.1503/cmaj.080148. PMC 2691438. PMID 19506281.
- ↑ Leighton, Patrick A; Koffi, Jules K; Pelcat, Yann; Lindsay, L Robbin; Ogden, Nicholas H (2012). «Predicting the speed of tick invasion: An empirical model of range expansion for the Lyme disease vector Ixodes scapularis in Canada». J. Appl. Ecol. 49 (2): 457–64. doi:10.1111/j.1365-2664.2012.02112.x.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (օգնություն) - ↑ Gordillo-Pérez G, Torres J, Solórzano-Santos F, de Martino S, Lipsker D, Velázquez E, Ramon G, Onofre M, Jaulhac B (October 2007). «Borrelia burgdorferi infection and cutaneous Lyme disease, Mexico». Emerging Infectious Diseases. 13 (10): 1556–8. doi:10.3201/eid1310.060630. PMC 2851501. PMID 18258006.
- ↑ 190,0 190,1 «Reported cases of Lyme disease by state or locality, 2005-2014†». cdc.gov. 2017-11-06. Արխիվացված է օրիգինալից 4 May 2012-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ «How many people get Lyme disease?». cdc.gov. Արխիվացված է օրիգինալից 13 October 2014-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ CDC (4 January 2012). «Reported Lyme disease cases by state, 2000-2010». Centers for Disease Control and Prevention (CDC). Արխիվացված է օրիգինալից 4 May 2012-ին. Վերցված է 29 April 2012-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Centers for Disease Control Prevention (CDC) (June 2007). «Lyme disease--United States, 2003-2005». MMWR. Morbidity and Mortality Weekly Report. 56 (23): 573–6. PMID 17568368. Արխիվացված է օրիգինալից 19 November 2012-ին.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Bacon RM, Kugeler KJ, Mead PS (October 2008). «Surveillance for Lyme disease--United States, 1992-2006». Morbidity and Mortality Weekly Report. Surveillance Summaries. 57 (10): 1–9. PMID 18830214. Արխիվացված է օրիգինալից 10 November 2012-ին.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ 195,0 195,1 Robbins, Jim (20 May 2003). «Montana Lab Tries to Identify Tick-Borne Disease». The New York Times. Արխիվացված է օրիգինալից 3 September 2017-ին.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ "Lyme Disease Data" Արխիվացված 30 Ապրիլ 2012 Wayback Machine. Centers for Disease Control and Prevention (CDC).
- ↑ «Lyme disease (Borrelia burgdorferi) 2011 case definition». U.S. Centers for Disease Control and Prevention. Արխիվացված է օրիգինալից 22 April 2012-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ 198,0 198,1 «Lyme disease (Borrelia burgdorferi) 2008 case definition». U.S. Centers for Disease Control and Prevention. Արխիվացված է օրիգինալից 12 June 2012-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ 199,0 199,1 Swanson KI, Norris DE (2007). «Detection of Borrelia burgdorferi DNA in lizards from Southern Maryland». Vector Borne and Zoonotic Diseases. 7 (1): 42–9. doi:10.1089/vbz.2006.0548. PMC 4128253. PMID 17417956.
- ↑ Richter D, Matuschka FR (July 2006). «Perpetuation of the Lyme disease spirochete Borrelia lusitaniae by lizards». Applied and Environmental Microbiology. 72 (7): 4627–32. doi:10.1128/AEM.00285-06. PMC 1489336. PMID 16820453.
- ↑ Giery ST, Ostfeld RS (June 2007). «The role of lizards in the ecology of Lyme disease in two endemic zones of the northeastern United States». The Journal of Parasitology. 93 (3): 511–7. doi:10.1645/GE-1053R1.1. PMID 17626342.
- ↑ Amore G, Tomassone L, Grego E, Ragagli C, Bertolotti L, Nebbia P, Rosati S, Mannelli A (March 2007). «Borrelia lusitaniae in immature Ixodes ricinus (Acari: Ixodidae) feeding on common wall lizards in Tuscany, central Italy». Journal of Medical Entomology. 44 (2): 303–7. doi:10.1603/0022-2585(2007)44[303:BLIIIR]2.0.CO;2. PMID 17427701.
- ↑ Majláthová V, Majláth I, Derdáková M, Víchová B, Pet'ko B (December 2006). «Borrelia lusitaniae and green lizards (Lacerta viridis), Karst Region, Slovakia». Emerging Infectious Diseases. 12 (12): 1895–901. doi:10.3201/eid1212.060784. PMC 3291370. PMID 17326941.
- ↑ Lyme disease fact sheet Analysis of CDC data on VoxHealth. Retrieved on 2013-30-1
- ↑ Mantovani E, Costa IP, Gauditano G, Bonoldi VL, Higuchi ML, Yoshinari NH (April 2007). «Description of Lyme disease-like syndrome in Brazil. Is it a new tick borne disease or Lyme disease variation?». Brazilian Journal of Medical and Biological Research = Revista Brasileira de Pesquisas Medicas e Biologicas. 40 (4): 443–56. doi:10.1590/S0100-879X2006005000082. PMID 17401487.
- ↑ Yoshinari NH, Oyafuso LK, Monteiro FG, de Barros PJ, da Cruz FC, Ferreira LG, Bonasser F, Baggio D, Cossermelli W (1993). «[Lyme disease. Report of a case observed in Brazil]» [Lyme disease. Report of a case observed in Brazil]. Revista do Hospital das Clinicas (Portuguese). 48 (4): 170–4. PMID 8284588.
{{cite journal}}: Unknown parameter|displayauthors=ignored (|display-authors=suggested) (օգնություն)CS1 սպաս․ չճանաչված լեզու (link) - ↑ Hoen AG, Margos G, Bent SJ, Diuk-Wasser MA, Barbour A, Kurtenbach K, Fish D (September 2009). «Phylogeography of Borrelia burgdorferi in the eastern United States reflects multiple independent Lyme disease emergence events». Proceedings of the National Academy of Sciences of the United States of America. 106 (35): 15013–8. Bibcode:2009PNAS..10615013H. doi:10.1073/pnas.0903810106. JSTOR 40484546. PMC 2727481. PMID 19706476.
{{cite journal}}: Unknown parameter|laydate=ignored (օգնություն); Unknown parameter|laysource=ignored (օգնություն); Unknown parameter|laysummary=ignored (օգնություն) - ↑ Josselyn, John (1670). An Account of Two Voyages to New-England Made during the Years 1638, 1663. Արխիվացված է օրիգինալից 25 June 2013-ին.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն)page 92 - ↑ 209,0 209,1 Drymon, MM (2008). Disguised as the devil: how Lyme disease created witches and changed history. էջեր 51–52. ISBN 978-0-615-20061-3.
- ↑ Summerton N (1995). «Lyme disease in the eighteenth century». BMJ. 311 (7018): 1478. doi:10.1136/bmj.311.7018.1478.
- ↑ Hall, Stephen S (November 2011). «Iceman Autopsy». National Geographic. Արխիվացված է օրիգինալից 19 October 2011-ին. Վերցված է 17 October 2011-ին.
{{cite magazine}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ 212,0 212,1 Marcus, Karl (1910). «Verhandlungen der dermatologischen Gesellschaft zu Stockholm». Arch. Dermatol. Syph. 101 (2–3): 403–06. doi:10.1007/BF01832773.
- ↑ Burckhardt JL (1911). «Zur Frage der Follikel- und Keimzentrenbildung in der Haut». Frankf. Z. Pathol. (German). 6: 352–59.
{{cite journal}}: CS1 սպաս․ չճանաչված լեզու (link) - ↑ Edlow, Jonathan A (2003). Bull's-eye: unraveling the medical mystery of Lyme disease. Yale University Press. ISBN 978-0-300-09867-9. page 191.
- ↑ Hellerström S (1930). «Erythema chronicum migrans Afzelii». Acta Derm.-Venerol. (German). 11: 315–21.
{{cite journal}}: CS1 սպաս․ չճանաչված լեզու (link) - ↑ Lenhoff C (1948). «Spirochetes in aetiologically obscure diseases». Acta Derm.-Venerol. 28: 295–324.
- ↑ Thyresson N (1949). «The penicillin treatment of acrodermatitis atrophicans chronica (Herxheimer)». Acta Dermato-Venereologica. 29 (6): 572–621. PMID 18140373.
- ↑ Bianchi GE (1950). «[Penicillin therapy of lymphocytoma]» [Penicillin therapy of lymphocytoma]. Dermatologica (German). 100 (4–6): 270–3. doi:10.1159/000257185. PMID 15421023.
{{cite journal}}: CS1 սպաս․ չճանաչված լեզու (link) - ↑ Paschoud JM (1954). «[Lymphocytoma after tick bite]» [Lymphocytoma after tick bite]. Dermatologica (German). 108 (4–6): 435–7. PMID 13190934.
{{cite journal}}: CS1 սպաս․ չճանաչված լեզու (link) - ↑ Scrimenti RJ (July 1970). «Erythema chronicum migrans». Archives of Dermatology. 102 (1): 104–5. doi:10.1001/archderm.102.1.104. PMID 5497158.
- ↑ Borchers AT, Keen CL, Huntley AC, Gershwin ME (February 2015). «Lyme disease: a rigorous review of diagnostic criteria and treatment». Journal of Autoimmunity. 57: 82–115. doi:10.1016/j.jaut.2014.09.004. PMID 25451629.
- ↑ Weir, William (19 September 2013). «Lyme Disease Pioneer Stephen Malawista Dies». Hartford Courant. Արխիվացված է օրիգինալից 14 October 2013-ին. Վերցված է 14 October 2013-ին.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Sternbach G, Dibble CL (1996). «Willy Burgdorfer: Lyme disease». The Journal of Emergency Medicine. 14 (5): 631–4. doi:10.1016/S0736-4679(96)00143-6. PMID 8933327.
- ↑ Bolognia JL, Jorizzo JL, Rapini RP (2007). Dermatology (2nd ed.). St. Louis: Mosby. ISBN 978-1-4160-2999-1.[Հղում աղբյուրներին]
- ↑ Mast WE, Burrows WM (November 1976). «Erythema chronicum migrans and "lyme arthritis"». JAMA. 236 (21): 2392d–2392. doi:10.1001/jama.236.21.2392d. PMID 989847.
- ↑ Steere AC, Malawista SE, Snydman DR, Shope RE, Andiman WA, Ross MR, Steele FM (1977). «Lyme arthritis: an epidemic of oligoarticular arthritis in children and adults in three connecticut communities». Arthritis and Rheumatism. 20 (1): 7–17. doi:10.1002/art.1780200102. PMID 836338.
- ↑ Steere AC, Hutchinson GJ, Rahn DW, Sigal LH, Craft JE, DeSanna ET, Malawista SE (July 1983). «Treatment of the early manifestations of Lyme disease». Annals of Internal Medicine. 99 (1): 22–6. doi:10.7326/0003-4819-99-1-22. PMID 6407378.
- ↑ Burgdorfer W (1984). «Discovery of the Lyme disease spirochete and its relation to tick vectors». The Yale Journal of Biology and Medicine. 57 (4): 515–20. PMC 2590008. PMID 6516454.
- ↑ Burgdorfer W, Barbour AG, Hayes SF, Benach JL, Grunwaldt E, Davis JP (June 1982). «Lyme disease-a tick-borne spirochetosis?». Science (Submitted manuscript). 216 (4552): 1317–9. Bibcode:1982Sci...216.1317B. doi:10.1126/science.7043737. PMID 7043737.
- ↑ Luft BJ, Volkman DJ, Halperin JJ, Dattwyler RJ (1988). «New chemotherapeutic approaches in the treatment of Lyme borreliosis». Annals of the New York Academy of Sciences. 539 (1): 352–61. Bibcode:1988NYASA.539..352L. doi:10.1111/j.1749-6632.1988.tb31869.x. PMID 3056203.
- ↑ Dattwyler RJ, Volkman DJ, Conaty SM, Platkin SP, Luft BJ (December 1990). «Amoxycillin plus probenecid versus doxycycline for treatment of erythema migrans borreliosis». Lancet. 336 (8728): 1404–6. doi:10.1016/0140-6736(90)93103-V. PMID 1978873.
- ↑ Ribeiro JM, Mather TN, Piesman J, Spielman A (March 1987). «Dissemination and salivary delivery of Lyme disease spirochetes in vector ticks (Acari: Ixodidae)». Journal of Medical Entomology. 24 (2): 201–5. PMID 3585913.
- ↑ LoGiudice K, Ostfeld RS, Schmidt KA, Keesing F (January 2003). «The ecology of infectious disease: effects of host diversity and community composition on Lyme disease risk». Proceedings of the National Academy of Sciences of the United States of America. 100 (2): 567–71. Bibcode:2003PNAS..100..567L. doi:10.1073/pnas.0233733100. PMC 141036. PMID 12525705.
- ↑ Patz JA, Daszak P, Tabor GM, Aguirre AA, Pearl M, Epstein J, Wolfe ND, Kilpatrick AM, Foufopoulos J, Molyneux D, Bradley DJ (July 2004). «Unhealthy landscapes: Policy recommendations on land use change and infectious disease emergence». Environmental Health Perspectives. 112 (10): 1092–8. doi:10.1289/ehp.6877. PMC 1247383. PMID 15238283.
- ↑ Khasnis AA, Nettleman MD (2005). «Global warming and infectious disease». Archives of Medical Research. 36 (6): 689–96. doi:10.1016/j.arcmed.2005.03.041. PMID 16216650.
- ↑ Feder HM, Johnson BJ, O'Connell S, Shapiro ED, Steere AC, Wormser GP, Agger WA, Artsob H, Auwaerter P, Dumler JS, Bakken JS, Bockenstedt LK, Green J, Dattwyler RJ, Munoz J, Nadelman RB, Schwartz I, Draper T, McSweegan E, Halperin JJ, Klempner MS, Krause PJ, Mead P, Morshed M, Porwancher R, Radolf JD, Smith RP, Sood S, Weinstein A, Wong SJ, Zemel L (October 2007). «A critical appraisal of "chronic Lyme disease"». The New England Journal of Medicine. 357 (14): 1422–30. doi:10.1056/NEJMra072023. PMID 17914043.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Halperin JJ, Shapiro ED, Logigian E, Belman AL, Dotevall L, Wormser GP, Krupp L, Gronseth G, Bever CT (July 2007). «Practice parameter: treatment of nervous system Lyme disease (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology». Neurology. 69 (1): 91–102. doi:10.1212/01.wnl.0000265517.66976.28. PMID 17522387.
- ↑ «"Chronic Lyme Disease" Fact Sheet». National Institute of Allergy and Infectious Diseases. 17 April 2009. Արխիվացված է օրիգինալից 15 December 2012-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ Marques A (June 2008). «Chronic Lyme disease: a review». Infectious Disease Clinics of North America. 22 (2): 341–60, vii–viii. doi:10.1016/j.idc.2007.12.011. PMC 2430045. PMID 18452806.
- ↑ 240,0 240,1 Little SE, Heise SR, Blagburn BL, Callister SM, Mead PS (April 2010). «Lyme borreliosis in dogs and humans in the USA». Trends in Parasitology. 26 (4): 213–8. doi:10.1016/j.pt.2010.01.006. PMID 20207198.
- ↑ 241,0 241,1 Krupka I, Straubinger RK (November 2010). «Lyme borreliosis in dogs and cats: background, diagnosis, treatment and prevention of infections with Borrelia burgdorferi sensu stricto». The Veterinary Clinics of North America. Small Animal Practice. 40 (6): 1103–19. doi:10.1016/j.cvsm.2010.07.011. PMID 20933139.
- ↑ Hahn, Jeffrey. «Ticks and Their Control». Regents of the University of Minnesota. Արխիվացված է օրիգինալից 25 February 2012-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն) - ↑ «Chronic Lyme Disease». National Institute of Allergy and Infectious Diseases. Արխիվացված է օրիգինալից 15 December 2012-ին. Վերցված է 15 October 2013-ին.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (օգնություն)
![]() Այս հոդվածը պարունակում է , աղբյուր՝ Centers for Disease Control and Prevention, փաստաթուղթ՝ "Post-Treatment Lyme Disease Syndrome".
Այս հոդվածը պարունակում է , աղբյուր՝ Centers for Disease Control and Prevention, փաստաթուղթ՝ "Post-Treatment Lyme Disease Syndrome".
Further reading
[խմբագրել | խմբագրել կոդը]- Richard Ostfeld (2012). Lyme Disease: The Ecology of a Complex System. New York: Oxford University Press. ISBN 978-0199928477.
- Pamela Weintraub (2008). Cure Unknown: Inside the Lyme Disease Epidemic. St. Martin's Press. ISBN 9780312378127.
External links
[խմբագրել | խմբագրել կոդը]Կաղապար:Medical condition classification and resources
| Վիքիպահեստ նախագծում կարող եք այս նյութի վերաբերյալ հավելյալ պատկերազարդում գտնել LianaYeghiazaryan/Ավազարկղ կատեգորիայում։ |
- Lyme disease organizations հոդվածը Curlie-ում (ըստ DMOZ-ի)
- CDC - Lyme Disease - NIOSH Workplace Safety and Health Topic: from the Centers for Disease Control and Prevention (CDC)
- Lyme Disease The Merck Manual
- Lyme Disease Tests - Lab Tests Online
- Tick-borne Diseases Passive Surveillance Public Database - Laboratory of Medical Zoology at the University of Massachusetts, Amherst
- Lyme Disease Map Project
Կաղապար:Tick-borne diseases Կաղապար:Gram-negative non-proteobacterial diseases Կաղապար:Arthritis in children
